Hong Kong Med J 2015 Dec;21(6):528–35 | Epub 16 Oct 2015
DOI: 10.12809/hkmj144457
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Early postoperative outcome of bipolar transurethral enucleation and resection of the prostate
CL Cho, FRCSEd (Urol), FHKAM (Surgery);
Clarence LH Leung, MRCSEd;
Wayne KW Chan, FRCSEd (Urol);
Ringo WH Chu, FRCSEd (Urol), FHKAM (Surgery);
IC Law, FRCSEd (Urol), FHKAM (Surgery)
Division of Urology, Department of Surgery, Kwong Wah Hospital, Yaumatei, Hong Kong
Corresponding author: Dr CL Cho (chochaklam@yahoo.com.hk)
Abstract
Objectives: To report the early
postoperative outcome of bipolar transurethral
enucleation and resection of the prostate. Our
results were compared with those published from
various centres.
Design: Case series.
Setting: Regional hospital, Hong Kong.
Patients: A total of 28 consecutive patients who had
undergone bipolar transurethral enucleation and
resection of the prostate by a single surgeon between
January and June 2014. All patients were evaluated
preoperatively by physical examination, digital
rectal examination, transrectal ultrasonography,
and laboratory studies, including measurement of
haemoglobin, sodium, and prostate-specific antigen
levels. Patients were assessed perioperatively and at
4 weeks and 3 months postoperatively.
Results: The mean resected specimen weight of
prostatic adenoma in 28 patients was 48.2 g with
a mean enucleation and resection time of 13.6
and 47.7 minutes, respectively. There was a mean
decrease in serum prostate-specific antigen by 85.9%
(from 6.4 ng/mL to 0.9 ng/mL) postoperatively.
Prostate volume was decreased by 68.2% (from
71.9 cm3 to 22.9 cm3) at 4 weeks postoperatively.
The mean postoperative haemoglobin drop was
11.5 g/L. The rate of transient urinary incontinence
at 3 months was 3.6%. Patients who underwent
bipolar transurethral enucleation and resection of
the prostate had a short catheterisation time and
hospital stay, which is comparable to conventional
transurethral resection of the prostate.
Conclusions: Bipolar transurethral enucleation
and resection of the prostate should become the
endourological equivalent to open adenomectomy
with fewer complications and short convalescence.
The technique of bipolar transurethral enucleation
and resection of the prostate can be acquired safely
with a relatively short learning curve.
New knowledge added by this study
- Bipolar transurethral enucleation and resection of the prostate (TUERP) achieves satisfactory early functional outcomes and is associated with low morbidity. The technique is applicable to prostates of all size.
- Outcomes comparable with large case series could be achieved with a short learning curve.
- Bipolar TUERP should be the technique of choice for a large-sized prostate.
- Bipolar TUERP is an alternative to conventional transurethral resection for small and medium-sized prostates.
Introduction
Despite the availability of numerous minimally
invasive techniques, transurethral resection of the
prostate (TURP) remains the most common surgical
treatment for lower urinary tract symptoms (LUTS)
caused by benign prostatic enlargement (BPE) in
small to medium-sized prostates.1 Nonetheless,
TURP has been associated with significant
complication rates.2
Bipolar TURP uses saline irrigation, which
decreases the risk of TURP syndrome compared
with monopolar TURP, and both bipolar and
monopolar TURP result in comparable functional
outcomes.3 The bipolar system can also be broadened
to enucleate the prostate gland along the surgical
capsule, using a resectoscope combined with a loop.
This transurethral enucleation and resection of the
prostate (TUERP) technique can potentially remove
more prostatic tissue than TURP and requires no
additional devices.
In the present study, we describe the technique
and early postoperative outcomes of bipolar TUERP
and compare our results with major international
series.
Methods
Patients
Between January 2014 and June 2014, 28 consecutive
patients underwent bipolar TUERP at Kwong Wah
Hospital, Hong Kong. All patients were evaluated
preoperatively by physical examination, digital
rectal examination, transrectal ultrasonography
(TRUS) of the prostate, and laboratory studies that
included measurement of haemoglobin, sodium,
and prostate-specific antigen (PSA). Patients were
offered the option of ultrasound-guided transrectal
prostate biopsy if the PSA level was >4 ng/mL or if
the digital rectal examination showed suspicion of
prostate cancer. Abnormal digital rectal examination
findings included prostate nodule, asymmetry of the
lateral lobes, or irregularity of the prostate. The TRUS
was performed to measure the maximum length,
width, and anteroposterior height of the prostate
to calculate the prostate volume using the ellipse
formula, where prostate volume (mL) = 0.52 x length
x width x height. Patient baseline characteristics,
indications for surgery, and operative data and
complications were recorded by doctors. Patients
with neurogenic bladder, previous genitourinary
tract surgery, urethral stricture, or known bladder
or prostate carcinoma were excluded from the
technique of bipolar TUERP.
Equipment and technique
All bipolar TUERP procedures were performed
by a single surgeon. This surgeon had performed
37 TUERPs using various techniques and devices
previously, before the procedure was standardised
as described below and shown in Figure 1. The
technique used in this report was first described by
and adopted from Prof CX Liu at Zhujiang Hospital
of Southern Medical University in Guangzhou.4
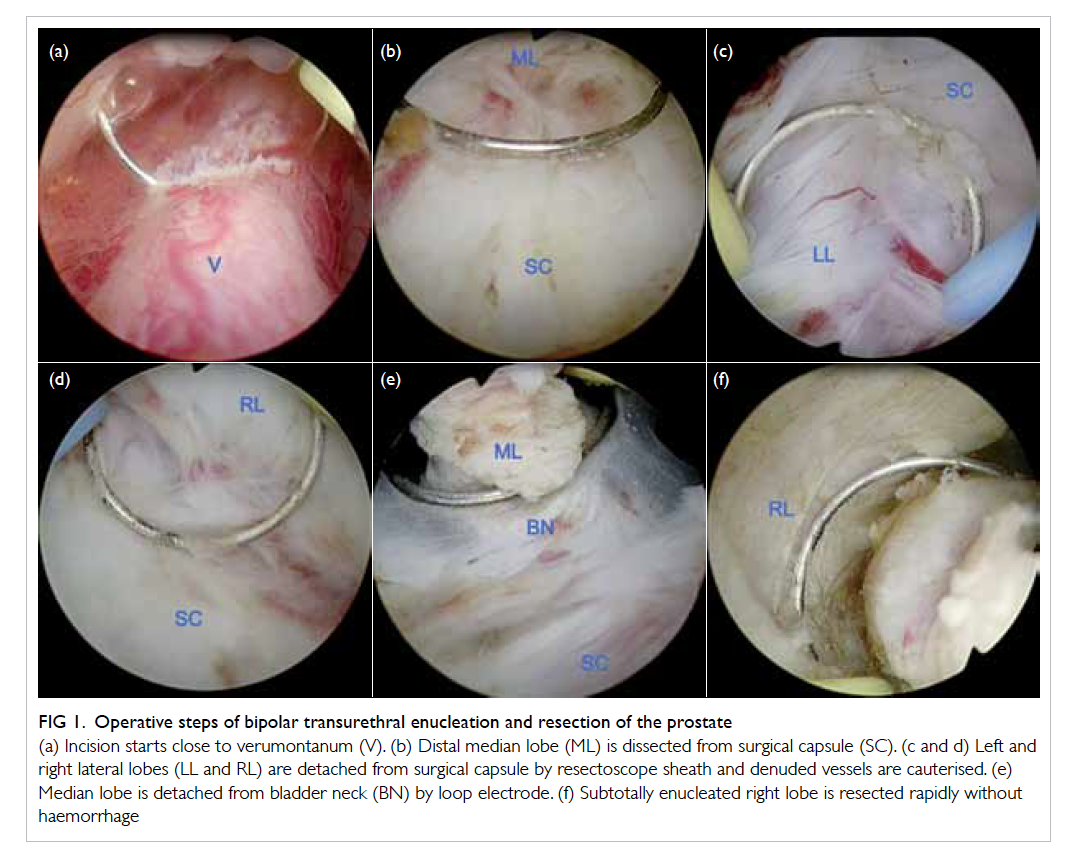
Figure 1. Operative steps of bipolar transurethral enucleation and resection of the prostate
(a) Incision starts close to verumontanum (V). (b) Distal median lobe (ML) is dissected from surgical capsule (SC). (c and d) Left and right lateral lobes (LL and RL) are detached from surgical capsule by resectoscope sheath and denuded vessels are cauterised. (e) Median lobe is detached from bladder neck (BN) by loop electrode. (f) Subtotally enucleated right lobe is resected rapidly without haemorrhage
Antiplatelet medications were stopped 3
days prior to surgery. Patients received general
or spinal anaesthesia and were placed in the
lithotomy position. Bladder stones where present
were fragmented with a holmium laser via a 21-Fr
rigid cystoscope and were evacuated with an Ellik
evacuator before bipolar TUERP. A 26-Fr Olympus
SurgMaster TURis resectoscope (Olympus Europe,
Hamburg, Germany) with a standard loop was used.
The incision was begun immediately proximal to the
verumontanum using a cutting current. The surgical
capsule plane was identified, and the whole gland
dissected in a retrograde fashion from the cleavage
plane using the resectoscope sheath, until the
circular fibres of the bladder neck were identified.
The loop electrode was used to coagulate all of the
denuded vessels immediately during the detachment
process. The adenoma was subtotally enucleated
with a narrow pedicle attached to the bladder neck at
the 6 o’clock position. The devascularised adenoma
was rapidly resected in pieces by the loop electrode.
The bladder neck at 5 to 7 o’clock was removed if
it appeared relatively high. The anterior commissure
at 12 o’clock was preserved except when it appeared
obstructive endoscopically. The chips were evacuated
with an Ellik evacuator. Finally, the prostatic fossa
was inspected and haemostasis secured. A 24-Fr
three-way urethral catheter was inserted at the end
of the procedure for bladder irrigation. One of the
patients in the series had open inguinal hernia repair
performed after bipolar TUERP. Haemoglobin level
and serum sodium concentration were measured
on the same day after surgery. The protocol for
postoperative care following bipolar TUERP was the
same as that for monopolar and bipolar TURP in our
unit. Bladder irrigation was stopped the following
morning, and the catheter was removed on the
second day postoperatively.
Follow-up
All patients were evaluated following bipolar TUERP
during clinic visits at 4 weeks and 3 months. At each
visit, history, physical examination, International
Prostate Symptom Score (IPSS), and TRUS of the
prostate were evaluated. The presence or absence
of transient urinary incontinence was documented
with direct questioning of the patient. Uroflowmetry
was performed at 8 weeks, and serum PSA levels
were measured at 3 months.
Results
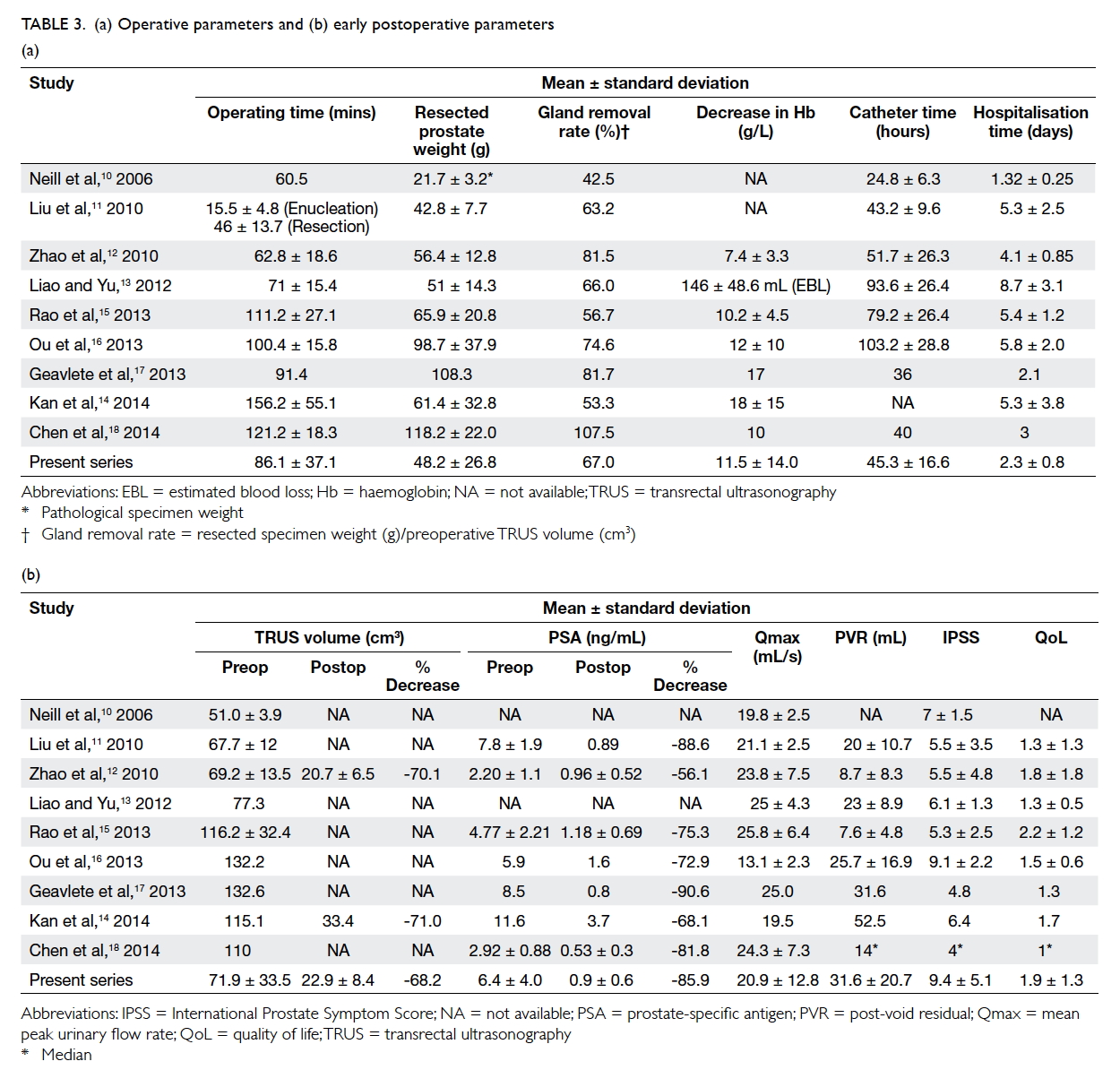
Table 1 lists the patients’ baseline characteristics,
operative data, and early postoperative outcomes.
Enucleation time was defined as the time from
incision to completion of subtotal enucleation
of the adenomatous tissue. Resection time was
defined as the time needed for fragmentation of the
en-bloc adenoma into chips. The mean enucleation
and resection times were 13.6 (median, 15; range,
10-30) minutes and 47.7 (median, 35; range, 15-120)
minutes, respectively, with a mean of 48.2 g of
adenoma resected.
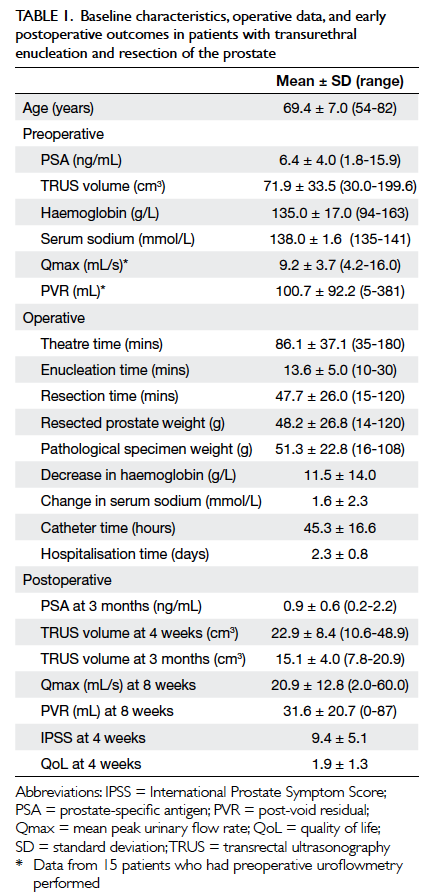
Table 1. Baseline characteristics, operative data, and early postoperative outcomes in patients with transurethral enucleation and resection of the prostate
The mean PSA level decreased from 6.4 ng/mL to
0.9 ng/mL at 3 months postoperatively, representing
an 85.9% decrease. Pathological examination of
enucleated tissue revealed prostatic adenocarcinoma
in one patient who had T1a disease with a Gleason
score of 6; the serum PSA level decreased from 4.6 ng/mL
to 1.7 ng/mL in this patient. There was a significant
decrease in mean TRUS volume from 71.9 cm3 to
22.9 cm3 at 4 weeks and to 15.1 cm3 at 3 months
postoperatively, corresponding to decreases of 68.2%
and 79.0% at 4 weeks and 3 months, respectively.
More than half of the patients in our series
(16 of 28 patients) presented with refractory acute
urinary retention or obstructive uropathy and
had required catheterisation prior to surgery.
Preoperative uroflowmetry within the last year
was available in only 15 patients, thus comparison
between preoperative and postoperative urodynamic
parameters was less representative. The mean peak
urinary flow rate was 20.9 mL/s, and the
mean post-void residual was 31.6 mL at 8 weeks
postoperatively. The mean IPSS was 9.4, and the mean
quality-of-life score was 1.9 at 4 weeks.
There was no requirement for blood
transfusion nor incidence of clot retention in any
patient. The mean decrease in haemoglobin was
11.5 g/L. Urinary tract infection presenting as acute
epididymitis was noted in two (7.1%) patients. One
(3.6%) patient required re-catheterisation on day 2
postoperatively and was successfully weaned off the
catheter on day 5. Transient urinary incontinence
was noted in three patients and one patient at 1 and 3 months
postoperatively, respectively (10.7% at 1 month and
3.6% at 3 months). An average of two incontinence
pads were required daily, and all cases of transient
urinary incontinence subsided within 4 months. No
urethral stricture, meatal stenosis, or bladder neck
contracture was noted at 3 months.
Discussion
The TURP has been considered the standard
surgical therapy for LUTS caused by BPE. Despite
improvements in equipment and techniques over
the years, TURP remains associated with significant
morbidity and re-treatment rates, particularly in
patients with a large prostate.5 Open prostatectomy
(OP) is therefore still considered a valid option for
patients with a prostate of >80 g.6
Surgical enucleation for the treatment of LUTS
caused by BPE remains the most complete method to
remove adenomas of any size; the history of surgical
enucleation dates back more than 100 years.7 In spite
of the low re-operation rate and high success rate,
OP is an invasive procedure associated with higher
transfusion rates, longer catheterisation time, and
longer hospital stay. As a result, the popularity of OP
has declined.
The concept of surgical enucleation was
revisited with the advent of endoscopic alternatives
to open enucleation. Endoscopic enucleation allows
for maximal removal of the adenoma and results in
potentially equivalent efficacy compared with its
open counterpart, with significantly lower morbidity.
Holmium laser enucleation of the prostate (HoLEP)
was the first endoscopic enucleative technique
described.8 This technique has been compared with
OP and TURP in various randomised controlled
trials, yielding at least comparable outcomes and
a favourable safety profile.9 The use of expensive
high-energy holmium laser equipment and a steep
learning curve, however, have limited the extensive
application of HoLEP worldwide. There has also
been a significant risk of bladder injury associated
with the use of the mechanical tissue morcellator
that is required for HoLEP.
The use of normal saline as an irrigant was
made possible by the introduction of bipolar devices.
As a result, the risk of TURP syndrome has been
virtually eliminated, and bipolar TURP has been
widely adopted for resection of larger prostates with
longer operating times. The use of a bipolar device
in endoscopic enucleation was first reported by Neill
et al,10 and bipolar TUERP requires no additional
devices in comparison with bipolar TURP. Moreover,
the sheath of the resectoscope is used for mechanical
enucleation of the adenoma along the plane of the
surgical capsule, instead of the holmium laser used
in HoLEP. The subtotally enucleated adenoma is then
resected into chips by the loop electrode, and the use
of a mechanical tissue morcellator is eliminated.
The nomenclature for this procedure has
not been standardised, with terms such as TUERP,
plasmakinetic enucleation of the prostate, and
bipolar plasma enucleation of the prostate reported
in the literature. All of these names generally refer
to the same procedure with minor differences. The
term ‘bipolar TUERP’ is used in this article.
Several modifications in technique and
equipment since the introduction of bipolar TUERP
have been suggested. For example, a spatula-like
enucleation loop, combined with a loop electrode
for haemostasis, was introduced by Olympus and is
especially designed for this procedure. Alternatively,
the use of thick loop electrodes and button electrodes
has been described in some series to facilitate the
enucleation process. Based on personal experience
with these different loops, the alternative loops with
different designs are generally stronger than the
conventional loop electrode, and they can be used
for mechanical enucleation without breakage. The
use of the loop in performing enucleation, instead of
the resectoscope sheath, also provides better, more
direct visualisation during the enucleation process
and potentially shortens the learning curve and
improves the safety of the procedure, particularly
in the early phase of learning. The resectoscope
sheath, however, facilitates a shorter enucleation
time without compromising safety with the
surgeon’s experience. The initial technique adopted
for bipolar TUERP was the ‘three-lobe’ technique.
This procedure starts with deep incisions down to
the surgical capsule at the 5 and 7 o’clock positions
from the bladder neck to the verumontanum, with
an additional incision at the 12 o’clock position
also reported. The median and lateral lobes of
the prostate are then subtotally enucleated and
resected in sequence. Some authors have reported
‘hybrid’ techniques, with the median lobe resected
as in conventional TURP and only the lateral lobes
enucleated. It has also been noted that deep incisions
might not be necessary, as the surgical capsule plane
can generally be identified with a small incision
immediately proximal to the verumontanum, and the
whole gland can be enucleated without separation
of the lobes. This procedure avoids the bleeding
associated with deep incisions of the bladder neck
and adenoma although a small lobe can sometimes
be difficult to enucleate after separation of the lobes.
The 12 o’clock incision has been mostly abandoned,
as has also been advocated for HoLEP. The anterior
commissure, particularly the distal part, has been
preserved to decrease the rate of transient urinary
incontinence postoperatively. The technique used
in our centre is currently the most widely practised
among different centres.
Several series have reported the perioperative
outcomes of bipolar TUERP using similar surgical
techniques. Only the largest series from each centre
was included for comparison; most of the published
series are from China. The results of our series were
compared with the TUERP arms of the various
published series; this list of series and a comparison
of the preoperative parameters are listed in Table 2. After the first published article by Neill et al10
comparing HoLEP and bipolar TUERP in 2006, Liu
et al11 published the largest series with 1600 patients
in 2010. Zhao et al12 and Liao and Yu13 followed by
comparing bipolar TUERP and TURP in medium-sized prostates. Kan et al14 compared bipolar TUERP and TURP in large prostates, and Rao et al,15 Ou
et al,16 Geavlete et al,17 and Chen et al18 compared
bipolar TUERP with OP. The operative and early
postoperative outcomes of bipolar TUERP from
various studies are listed in Table 3.
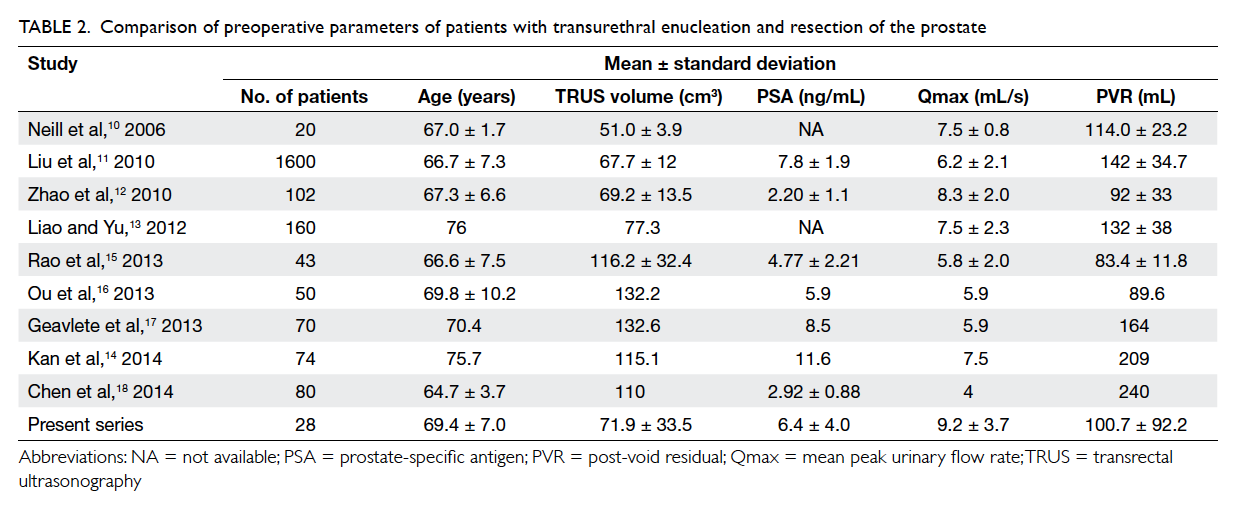
Table 2. Comparison of preoperative parameters of patients with transurethral enucleation and resection of the prostate
The operating time was generally longer
when the preoperative TRUS volume and resected
prostate weight increased. Although Liu et al11
reported enucleation and resection times without
reporting the total operating time, the preoperative
TRUS volume and resected prostate weight were
comparable between Liu et al’s report11 and
our series. In addition, the resection time was
prostate-size–dependent, and a resection efficacy of
approximately 1 g/min was reported in both Liu et
al’s report11 and our series. The enucleation time was
less size-dependent, varying from 10 to 30 minutes,
despite the large range of prostate sizes in our series.
The decrease in haemoglobin of approximately
10 g/L was reported for both medium-sized and large
prostates. Early control of denuded vessels during
the enucleation process made the removal of large
glands possible, with minimal blood loss during the
resection process.
The catheterisation and hospitalisation times
varied greatly among the series evaluated. Longer
times for both have typically been reported in series
from China.11 12 13 15 16 18 In addition, no standard protocols
were stated in most of the series, and the decision
for catheter removal and hospital discharge were
at the discretion of the surgeons. We report short
catheterisation and hospitalisation times with the
adoption of the same protocol as TURP in our
institution. Specifically, bladder irrigation was
stopped on postoperative day 1, the catheter was
removed, and the patient was discharged from the
hospital on postoperative day 2. A total of 92.9% of
the patients (26 of 28 patients) complied with the
postoperative protocol.
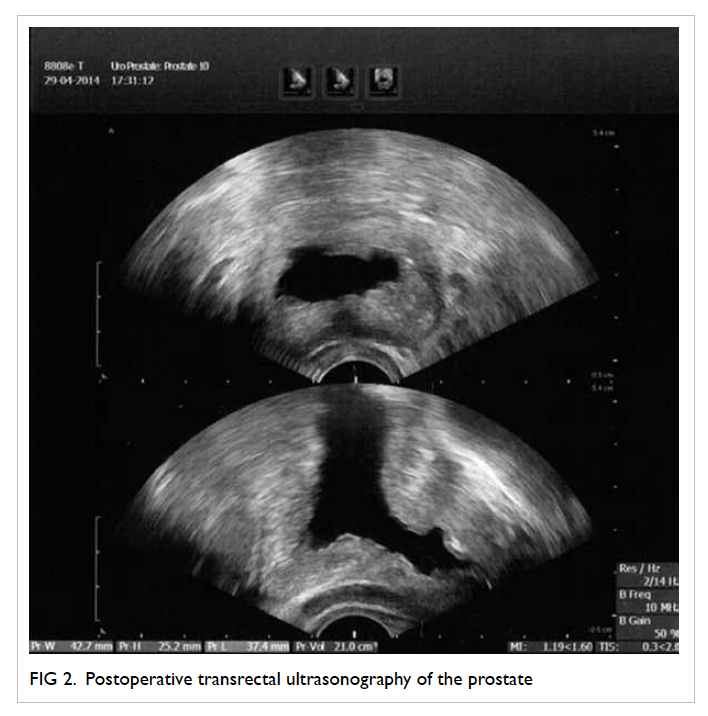
Postoperative TRUS volume was rarely reported
by the series despite the consistent reporting of
preoperative volume. This lack of reporting reflects
the difficulty in accurately estimating residual tissue
volume by TRUS, as illustrated by the postoperative
TRUS photo shown in Figure 2. In addition, the central cavity remaining after TUERP can lead
to overestimation of the prostate volume with
the application of the traditional ellipse formula.
Instead, preoperative estimation of the peripheral
zone volume, obtained by subtracting the volume
of the central zone from the total prostate volume,
may represent a better method for estimating the
residual tissue volume after TUERP. A decrease in
TRUS volume of approximately 70% after TUERP
was consistently reported, despite the pitfalls of
postoperative TRUS measurements.
It has also been shown from the experience of
HoLEP that a reduction in PSA level correlated with the
amount of prostate tissue removed.19 Thus, serum
PSA may serve as a better surrogate marker in the
estimation of postoperative residual tissue volume.
A postoperative PSA level of approximately 1 ng/mL
and a decrease in PSA by >70% were commonly
reported in most of the series.
Adverse events were poorly and inconsistently
reported, as shown in Table 4. The standard Clavien classification was not adopted. There was no
Clavien grade 3 or 4 complication in our series. The
transfusion rate was low, with the exception of the
series by Ou et al,16 and clot retention was rare. The
rate of urinary tract infection ranged from 2% to
7.3%, and the re-catheterisation rate was <5%. Major
complications were not common but did occur, as
reported by Kan et al14; four admissions to intensive
care units and nine conversions to other procedures
were reported in this series of 74 patients. The rate
of urethral stricture or bladder neck stenosis was low
and comparable with conventional TURP as reported
by the series by Liu et al.11 Long-term outcome was
not reported in our series due to the short duration
of follow-up. Temporary urinary incontinence was
the major concern with enucleative procedures, and
OP resulted in temporary urinary incontinence in
approximately 10% of cases. The reporting of transient
urinary incontinence after TUERP was poor and
did not feature in three of the nine series analysed.
Furthermore, the definition, timing, and severity of
urinary incontinence were not stated in the other
studies. Dramatic changes in the symptomatology of
the patients over time following benign prostatic hyperplasia–related surgery,
however, likely explain the difficulty in defining
transient urinary incontinence. In our experience,
transient urinary incontinence is not uncommon
after TURP, although it is difficult to differentiate the
type of urinary incontinence, stress, urge or mixed,
by history or urodynamic studies. The natural history
of this phenomenon has rarely been reported in the
literature. It was interesting to note that the rate of
transient urinary incontinence was much higher for
the TURP group (16.1%) compared with the TUERP
group (7.5%) in the series by Liao and Yu.13 In our
experience, 17.9% of patients reported episode(s) of
urinary incontinence at any time point after TUERP;
the rate of transient urinary incontinence was
10.7% and 3.6% at 1 and 3 months postoperatively,
respectively. Patients who had transient urinary
incontinence used two pads daily on average, and all
cases of transient urinary incontinence subsided by
4 months. Further investigations with, for example,
measurement of pad weight and urodynamic studies
will better delineate the cause and natural history of
postoperative transient urinary incontinence. There
is currently no predictive factor identified for the
phenomenon.
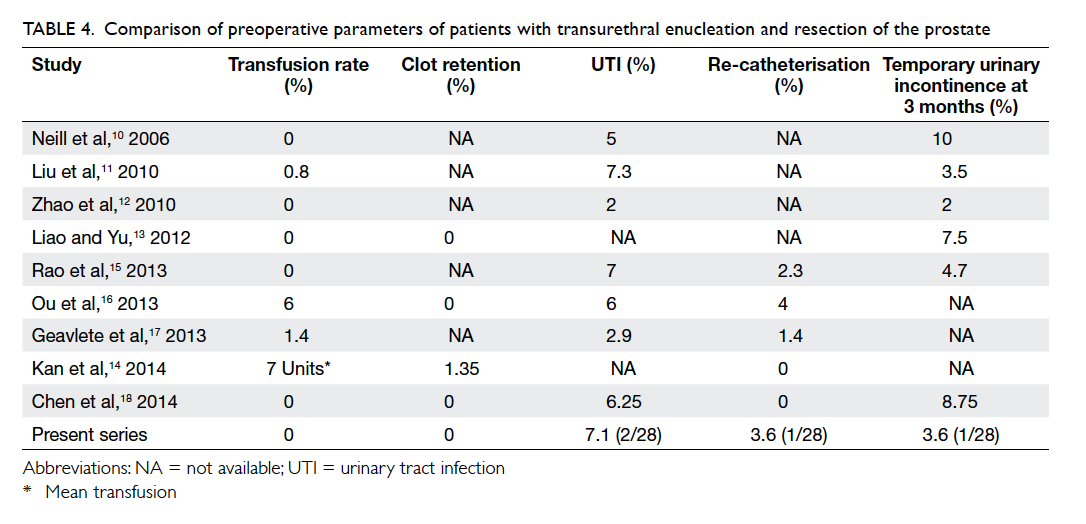
Table 4. Comparison of preoperative parameters of patients with transurethral enucleation and resection of the prostate
Comparison of outcome and complications
between patients with and without urinary retention
was limited by the small patient number in our study.
No significant difference between outcome and
complications was identified even though patients
with retention were significantly older.
A learning curve of 50 cases was reported for
HoLEP,20 and this learning curve was expected to
be shorter for bipolar TUERP. The instrumentation
for TUERP should be familiar to an endourologist
experienced in TURP because no additional devices
are required. Xiong et al21 analysed the learning
curve of bipolar TUERP. The ratio of conversion to
conventional TURP decreased after 30 cases, and
the efficiency of enucleation and resection increased
with accumulative experience after 50 cases. Our
series showed that the early postoperative outcomes
were comparable to those of large series after
approximately 35 cases, without an increase in
adverse events. The findings were based on analysis
of the learning curve of a single surgeon and may
not be applicable to all surgeons. Nevertheless, an
estimation of a learning curve in a magnitude of 30
to 50 cases seems reasonable and serves as a valuable
reference.
Conclusions
Our study suggests that bipolar TUERP is a safe
technique for prostates of any size. This procedure
should become the endourological equivalent to
open adenomectomy, with fewer complications and
shorter convalescence. This technique can also be
acquired safely with a relatively short learning curve.
References
1. AUA Practice Guidelines Committee. AUA guideline
on management of benign prostatic hyperplasia (2003).
Chapter 1: Diagnosis and treatment recommendations. J
Urol 2003;170:530-47. Crossref
2. Madersbacher S, Lackner J, Brössner C, et al. Reoperation,
myocardial infarction and mortality after transurethral and
open prostatectomy: a nation-wide, long-term analysis of
23,123 cases. Eur Urol 2005;47:499-504. Crossref
3. Mamoulakis C, Ubbink DT, de la Rosette JJ. Bipolar
versus monopolar transurethral resection of the prostate:
a systematic review and meta-analysis of randomized
controlled trials. Eur Urol 2009;56:798-809. Crossref
4. Liu C, Zheng S, Li H, Xu K. Transurethral enucleative
resection of prostate for treatment of BPH. Eur Urol 2006;5
Suppl:234. Crossref
5. Rassweiler J, Teber D, Kuntz R, Hofmann R. Complications
of transurethral resection of the prostate (TURP)—incidence, management, and prevention. Eur Urol
2006;50:969-79; discussion 980. Crossref
6. Oelke M, Bachmann A, Descazeaud A, et al. EAU guidelines
on the treatment and follow-up of non-neurogenic male
lower urinary tract symptoms including benign prostatic
obstruction. Eur Urol 2013;64:118-40. Crossref
7. Freyer PJ. Total enucleation of the prostate. A further series
of 550 cases of the operation. Br Med J 1919;1:121-120.2.
8. Gilling PJ, Kennett KM, Fraundorfer MR. Holmium laser
enucleation of the prostate for glands larger than 100
g: an endourologic alternative to open prostatectomy. J
Endourol 2000;14:529-31. Crossref
9. Ahyai SA, Gilling P, Kaplan SA, et al. Meta-analysis
of functional outcomes and complications following
transurethral procedures for lower urinary tract symptoms
resulting from benign prostatic enlargement. Eur Urol
2010;58:384-97. Crossref
10. Neill MG, Gilling PJ, Kennett KM, et al. Randomized trial
comparing holmium laser enucleation of prostate with
plasmakinetic enucleation of prostate for treatment of
benign prostatic hyperplasia. Urology 2006;68:1020-4. Crossref
11. Liu C, Zheng S, Li H, Xu K. Transurethral enucleation
and resection of prostate in patients with benign prostatic
hyperplasia by plasma kinetics. J Urol 2010;184:2440-5. Crossref
12. Zhao Z, Zeng G, Zhong W, Mai Z, Zeng S, Tao X. A
prospective, randomised trial comparing plasmakinetic
enucleation to standard transurethral resection of the
prostate for symptomatic benign prostatic hyperplasia:
three-year follow-up results. Eur Urol 2010;58:752-8. Crossref
13. Liao N, Yu J. A study comparing plasmakinetic enucleation
with bipolar plasmakinetic resection of the prostate for
benign prostatic hyperplasia. J Endourol 2012;26:884-8. Crossref
14. Kan CF, Tsu HL, Chiu Y, To HC, Sze B, Chan SW.
A prospective study comparing bipolar endoscopic
enucleation of prostate with bipolar transurethral resection
in saline for management of symptomatic benign prostate
enlargement larger than 70 g in a matched cohort. Int Urol
Nephrol 2014;46:511-7. Crossref
15. Rao JM, Yang JR, Ren YX, He J, Ding P, Yang JH.
Plasmakinetic enucleation of the prostate versus
transvesical open prostatectomy for benign prostatic
hyperplasia >80 mL: 12-month follow-up results of a
randomized clinical trial. Urology 2013;82:176-81. Crossref
16. Ou R, Deng X, Yang W, Wei X, Chen H, Xie K. Transurethral
enucleation and resection of the prostate vs transvesical
prostatectomy for prostate volumes >80 mL: a prospective
randomized study. BJU Int 2013;112:239-45. Crossref
17. Geavlete B, Stanescu F, Iacoboaie C, Geavlete P. Bipolar
plasma enucleation of the prostate vs open prostatectomy
in large benign prostatic hyperplasia cases—a medium
term, prospective, randomized comparison. BJU Int
2013;111:793-803. Crossref
18. Chen S, Zhu L, Cai J, et al. Plasmakinetic enucleation of the
prostate compared with open prostatectomy for prostates
larger than 100 grams: a randomized noninferiority
controlled trial with long-term results at 6 years. Eur Urol
2014;66:284-91. Crossref
19. Tinmouth WW, Habib E, Kim SC, et al. Change in serum
prostate specific antigen concentration after holmium laser
enucleation of the prostate: a marker for completeness of
adenoma resection? J Endourol 2005;19:550-4. Crossref
20. Shah HN, Mahajan AP, Sodha HS, Hegde S, Mohile PD,
Bansal MB. Prospective evaluation of the learning curve
for holmium laser enucleation of the prostate. J Urol
2007;177:1468-74. Crossref
21. Xiong W, Sun M, Ran Q, Chen F, Du Y, Dou K. Learning
curve for bipolar transurethral enucleation and resection
of the prostate in saline for symptomatic benign prostatic
hyperplasia: experience in the first 100 consecutive
patients. Urol Int 2013;90:68-74. Crossref