Hong Kong Med J 2015 Oct;21(5):475.e1–2
DOI: 10.12809/hkmj154526
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Endophthalmitis caused by Bacillus cereus: a devastating ophthalmological emergency
KC Lam, MB, BS, FRCR
Department of Radiology, Queen Mary Hospital, Pokfulam, Hong Kong
Corresponding author: Dr KC Lam (kclammbbs@gmail.com)
A 79-year-old man with lymphoma was admitted
for chemotherapy in November 2014. During his
admission, he complained of acute onset of left eye
pain with loss of vision. There was no history of
previous eye disease or injury.
On examination, his left eye had no light
perception and intra-ocular pressure was raised to
more than 50 mm Hg. There was left eye proptosis,
chemosis, and oedema over the eyelid. There was no
fundal view. B-scan performed by the ophthalmologist
showed increased vitreous echogenicity. A complete
blood picture showed low levels of haemoglobin (104
g/L) and thrombocytopenia (13 x 109 /L), and total
white cell count reduced to 0.69 x 109 /L. Blood was
taken from the central line for culture. Computed
tomographic scan of the orbit was performed to look
for intra-orbital haematoma as the platelet level
was low. Computed tomographic scan showed left
proptosis, left eyelid swelling, and increased soft
tissue stranding in the retro-ocular space (Fig 1). The lens was dislocated into the posterior chamber
and the density of vitreous humour was increased
when compared with the right globe. The difference
in densities between the two globes was exaggerated
at a follow-up scan 6 hours later (Fig 2). Overall radiological findings were compatible with severe
inflammation of the globe with pus in the posterior
chamber complicated by lens dislocation. The patient
was diagnosed with endophthalmitis and antibiotic
treatment was started. The patient began to have
pustular discharge from a ruptured corneal ulcer and
subsequent evisceration of the eye was required. The
specimen and the initial blood culture were positive
for Bacillus species. The organism was sensitive for
vancomycin and gentamicin.
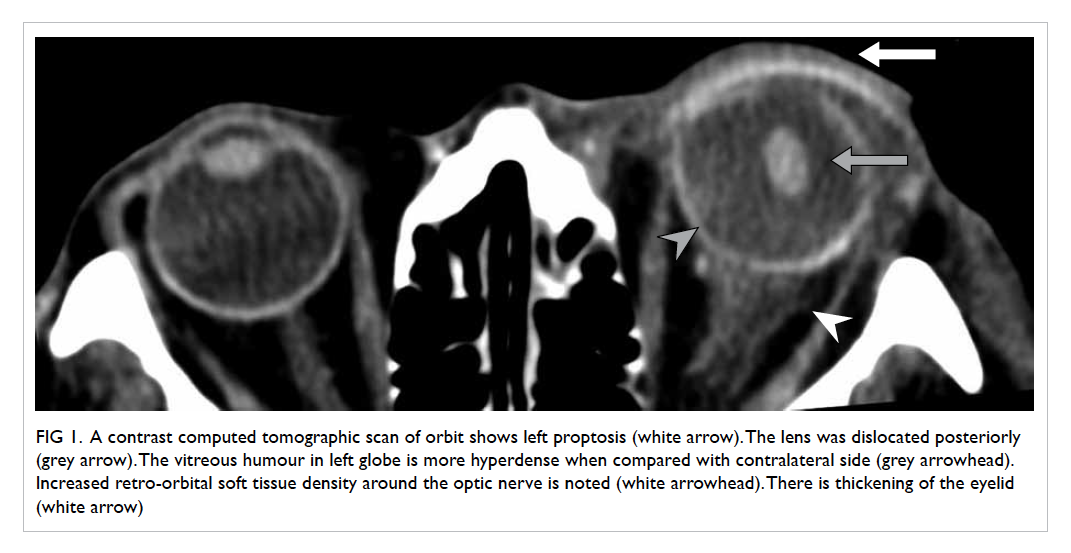
Figure 1. A contrast computed tomographic scan of orbit shows left proptosis (white arrow). The lens was dislocated posteriorly (grey arrow). The vitreous humour in left globe is more hyperdense when compared with contralateral side (grey arrowhead). Increased retro-orbital soft tissue density around the optic nerve is noted (white arrowhead). There is thickening of the eyelid (white arrow)
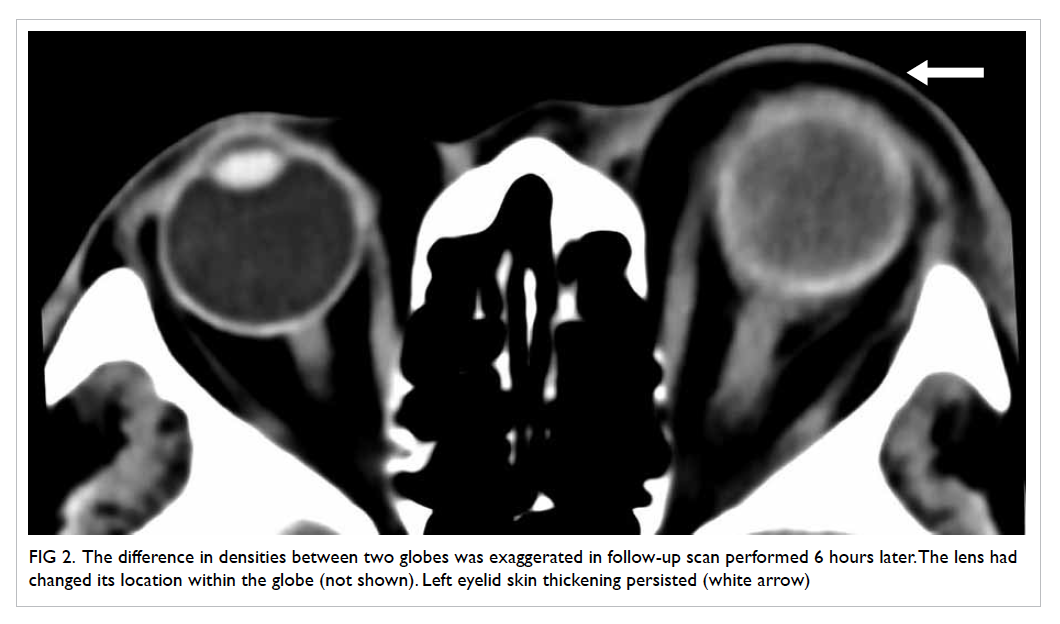
Figure 2. The difference in densities between two globes was exaggerated in follow-up scan performed 6 hours later. The lens had changed its location within the globe (not shown). Left eyelid skin thickening persisted (white arrow)
Endophthalmitis can be classified broadly into
endogenous or exogenous and can cause permanent
blindness. Exogenous endophthalmitis is usually due
to trauma or postoperative infection. Endogenous
endophthalmitis is commonly due to bacteraemia and
immunocompromised patients are at particular risk.
Endogenous endophthalmitis is relatively
uncommon, accounting for 2% to 8% of all
endophthalmitis cases. Staphylococcus aureus,
Bacillus cereus, Escherichia coli, Neisseria
meningitidis, and Klebsiella are common pathogens.1
Bacillus cereus is a highly virulent organism as it
can produce toxins that trigger severe intra-ocular
inflammation and can cause complete loss of vision
or destruction of the globe within 24 to 48 hours.1 2
Patients may end up with enucleation and permanent
loss of vision. Intravenous drug abusers are prone to
Bacillus infection.3 The cause of Bacillus infection
in our patient was unknown although the central
venous catheter was a potential culprit.
This article illustrates the radiological features
of endophthalmitis. It is usually a clinical diagnosis
although imaging may be required in complicated
cases. The prognosis for Bacillus endophthalmitis is
poor despite vigorous treatment.
References
1. Callegan MC, Engelbert M, Parke DW 2nd, Jett BD,
Gilmore MS. Bacterial endophthalmitis: epidemiology,
therapeutics, and bacterium-host interactions. Clin
Microbiol Rev 2002;15:111-24. Crossref
2. Kumar N, Garg N, Kumar N, Van Wagoner N. Bacillus
cereus panophthalmitis associated with injection drug use.
Int J Infect Dis 2014;26:165-6. Crossref
3. Hatem G, Merritt JC, Cowan CL Jr. Bacillus cereus
panophthalmitis after intravenous heroin. Ann
Ophthalmol 1979;11:431-40.

