Hong Kong Med J 2015 Oct;21(5):435–43 | Epub 15 Sep 2015
DOI: 10.12809/hkmj144385
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Intensive care unit family satisfaction survey
SM Lam, MB, BS, FHKAM (Medicine)1;
HM So, MN, MSc1;
SK Fok, MN1;
SC Li, RN, MN1;
CP Ng, BSN1;
WK Lui, RN1;
DK Heyland, MSc, MD2;
WW Yan, MB, BS, FHKAM (Medicine)1
1 Department of Intensive Care, Pamela Youde Nethersole Eastern Hospital, Chai Wan, Hong Kong
2 Department of Medicine, Queen’s University, Kingston, Ontario, Canada
 Full
paper in PDF
Full
paper in PDF
Corresponding author: Dr SM Lam (lamsm2@ha.org.hk)
Abstract
Objectives: To examine the level of family satisfaction
in a local intensive care unit and its performance in
comparison with international standards, and to
determine the factors independently associated with
higher family satisfaction.
Design: Questionnaire survey.
Setting: A medical-surgical adult intensive care unit
in a regional hospital in Hong Kong.
Participants: Adult family members of patients
admitted to the intensive care unit for 48 hours or
more between 15 June 2012 and 31 January 2014,
and who had visited the patient at least once during
their stay.
Results: Of the 961 eligible families, 736
questionnaires were returned (response rate, 76.6%).
The mean (± standard deviation) total satisfaction
score, and subscores on satisfaction with overall
intensive care unit care and with decision-making
were 78.1 ± 14.3, 78.0 ± 16.8, and 78.6 ± 13.6,
respectively. When compared with a Canadian
multicentre database with respective mean scores of
82.9 ± 14.8, 83.5 ± 15.4, and 82.6 ± 16.0 (P<0.001),
there was still room for improvement. Independent
factors associated with complete satisfaction with
overall care were concern for patients and families,
agitation management, frequency of communication by nurses, physician skill and competence, and
the intensive care unit environment. A performance-importance
plot identified the intensive care unit
environment and agitation management as factors
that required more urgent attention.
Conclusions: This is the first intensive care unit
family satisfaction survey published in Hong Kong.
Although comparable with published data from
other parts of the world, the results indicate room
for improvement when compared with a Canadian
multicentre database. Future directions should focus
on improving the intensive care unit environment,
agitation management, and communication with
families.
New knowledge added by this
study
- This study provides the first dataset on the level of family satisfaction with intensive care unit (ICU) care in Hong Kong.
- Factors that independently affected family satisfaction include the ICU environment, agitation management, and communication between health care workers and families. These are all potentially amenable to improvement.
- Factors identified to be independently associated with higher family satisfaction will provide directions for future improvement.
- Such baseline data will allow for assessment of the efficacy of future improvement initiatives.
Introduction
Providing professional care and establishing a good
rapport with patients is the mission of all health
care workers. This relationship building is part
of the patient-centred health care delivery model
that is currently being advocated over a clinician- or
disease-centred model.1 It is associated with
better clinical outcomes and may reduce potential
complaints due to miscommunication.2 3 4 In the intensive care setting where patients often cannot
make their own decisions, either due to their illness
or to the effect of medications,5 building a good
relationship with the patients’ family is especially
important. Furthermore, it has been recognised that
families of patients admitted to the intensive care
unit (ICU) are at higher risk of developing anxiety,
depression, and post-traumatic stress disorder.6 7
They are suddenly subjected to an uncertain outcome
for their loved ones, with associated emotional,
social and financial consequences, and in a strange
environment packed with complex technological
advancements. The long-term psychological impact
on the family after an ICU encounter is now termed
as post-intensive care syndrome–family (PICS-F).7
This adds to the society’s health care burden and
reduces the family ability to provide care. Evidence
suggests that the risk of developing PICS-F is
affected by the manner in which health care workers
interact with the family.8 For these reasons, ICU
quality measurement should include the families’
perspective and their satisfaction with the care
process.9 10
In early 2012, the Department of Intensive
Care, Pamela Youde Nethersole Eastern Hospital,
Hong Kong (PYNICU) initiated the Family
Satisfaction Enhancement (FAME) programme
that aimed to improve family satisfaction with ICU
care. A regular satisfaction survey was performed
that intended to identify problem areas and make
subsequent improvements. The current study was
part of the FAME programme that evaluated the level
of family satisfaction in a local ICU and its performance
in comparison with international standards, and
determined factors that are independently associated
with a higher family satisfaction and could be used to
plan future initiatives.
Methods
This was a questionnaire survey carried out at
PYNICU, which is a mixed medical-surgical 22-bed
adult ICU in a regional hospital with 1633 beds
in Hong Kong. It is a closed ICU with 24-hour
intensivist coverage.
The Family Satisfaction in the ICU (FS-ICU)
questionnaire is a patient family satisfaction
questionnaire originally developed in 2003 by a
group of health care professionals in Canada: the
Canadian Researchers at the End of Life Network
(CARENET).5 The questionnaire has been validated
for use in North America and Europe,11 12 13 14 and has
been translated into other languages including
Chinese. The questionnaire is accessible online
(http://www.thecarenet.ca). The questionnaire
consists of 37 items in two parts: satisfaction with
overall ICU care, and satisfaction with decision-making
around the care of critically ill patients; and
three open-ended questions. Respondents were
asked to provide baseline data (sex, age, relationship
with the patient, prior experience with ICU, and
whether they lived together before admission) at the
start of the questionnaire. Corresponding patient
data were retrieved from the Clinical Management
System, electronic Patient Record, and Clinical Data
Analysis and Reporting System.
Patients who were admitted to the ICU for 48
hours or more between 15 June 2012 and 31 January
2014, and were visited by their next-of-kin (NOK;
defined as the key contact person nominated by
the family and documented on the nursing chart on
admission) during their stay in the ICU were eligible.
Once an eligible patient was nearing ICU discharge
(defined as an expected date of ICU discharge
within the next 5 days as judged each morning
by a senior clinician or nurse consultant), or had
passed away in the ICU, his/her NOK was invited
by an independent research assistant not involved in
clinical care to participate in the survey. A minimum
stay of 48 hours was used as in previous studies
to ensure an adequate exposure of families to the
ICU.15 16 A copy of the questionnaire and an envelope were given to the NOK to be completed based on
his/her opinion. He/she was asked to return the
questionnaire in the envelope provided, which was
opened only by researchers. Those who failed to
return the questionnaire were contacted by phone
within 2 months of ICU discharge or death, and
the questionnaire was sent to them with a stamped
addressed envelope if they agreed to participate. All
respondents were ensured of the confidentiality and
anonymity of their response. For patients who were
admitted to the ICU more than once within the same
hospitalisation, only the last was analysed.
The study protocol was reviewed by the Hong
Kong East Cluster Ethics Committee and the need
for consent was waived.
Statistical analyses
Items in the FS-ICU questionnaire were scored as previously
described12: each item was recoded into a linear
scale ranging from 0 to 100, with 0 as very poor or
very dissatisfied, and 100 as excellent or completely
satisfied. Three items (“received appropriate amount
of information”, “had enough time to think in decision-making
process”, and “adequate time to address
concerns and answer questions”) were recoded into
dichotomous variables, while two items (“involved
at right time in decision-making process”, and “given
right amount of hope patient would recover”) were
recoded into a 3-point Likert scale.12 A mean (± standard
deviation [SD]) score was computed for each item.
Subscores for satisfaction with overall ICU care
(FS-ICU/Care) and satisfaction with role in decision-making
(FS-ICU/DM), and a total score (FS-ICU/Total) were generated by averaging available items,
provided that the respondent answered 70% or more
of the items in the respective sections.12
Results were compared using Mann-Whitney
U test with those of a multicentre Canadian database
(written communication, Daren Heyland, Feb 2014) that comprised data captured
from 2003 to 2006 at 12 Canadian sites.
Univariate analyses of satisfaction with overall
ICU care and satisfaction with role in decision-making
were conducted. Variables included the
baseline respondent’s and patient’s characteristics,
as well as items of part 1 or part 2 of FS-ICU,
respectively. Continuous variables were categorised
using their median, and questionnaire items were
categorised into “completely satisfied” and “less than
completely satisfied”. Factors with a P value of ≤0.1
were entered into multivariable logistic regression
using stepwise backward elimination to identify
independent factors associated with complete
family satisfaction with overall ICU care and role in
decision-making.
The independent factors thus identified by
multivariable logistic regression were used in the
construction of performance-importance plots to
identify those factors that deserve more urgent
attention because of their higher importance
(regression weights above the median) but lower
performance (percentage of that item being rated as
“excellent” being below the median).
By applying the rule of 10 on logistic regression
analysis of family satisfaction with overall ICU care,
a target sample size was estimated to be 725 with
29 covariates with an estimated 40% of respondents
being “completely satisfied” with overall care. All tests
were two-sided, and a P value of <0.05 was considered
statistically significant. All data were analysed
using the Statistical Package for the Social Sciences
(Windows version 20; SPSS Inc, Chicago [IL], US).
Results
From 15 June 2012 to 31 January 2014, 961 patients
were eligible and 822 families agreed to participate;
736 questionnaires were eventually returned,
with a response rate of 76.6%. Excluding the three
questions only applicable to families of patients
who passed away in ICU and the three open-ended
questions, 23 766 (95.0%) of the total 25 024
questions were completed. Baseline characteristics
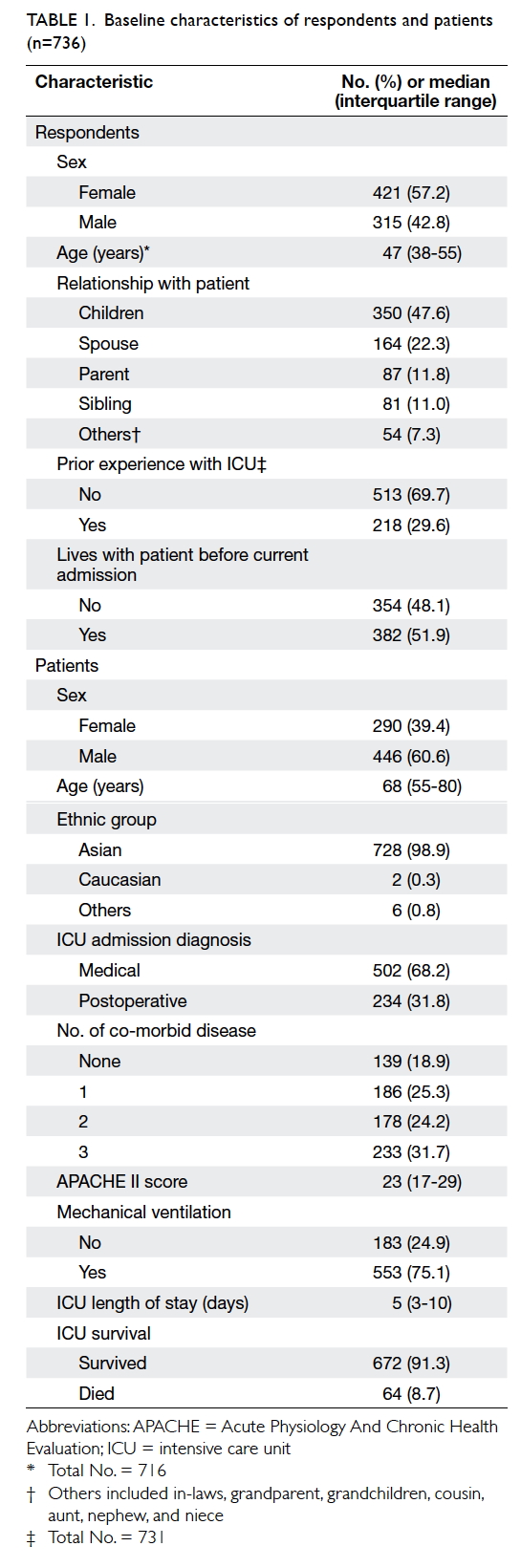
of the respondents and patients are shown in Table 1.
Our mean (± SD) FS-ICU/Total, FS-ICU/Care,
and FS-ICU/DM scores were 78.1 ± 14.3, 78.0 ±
16.8, and 78.6 ± 13.6, respectively. Table 2 shows the percentage of responses and mean score for each
questionnaire item.
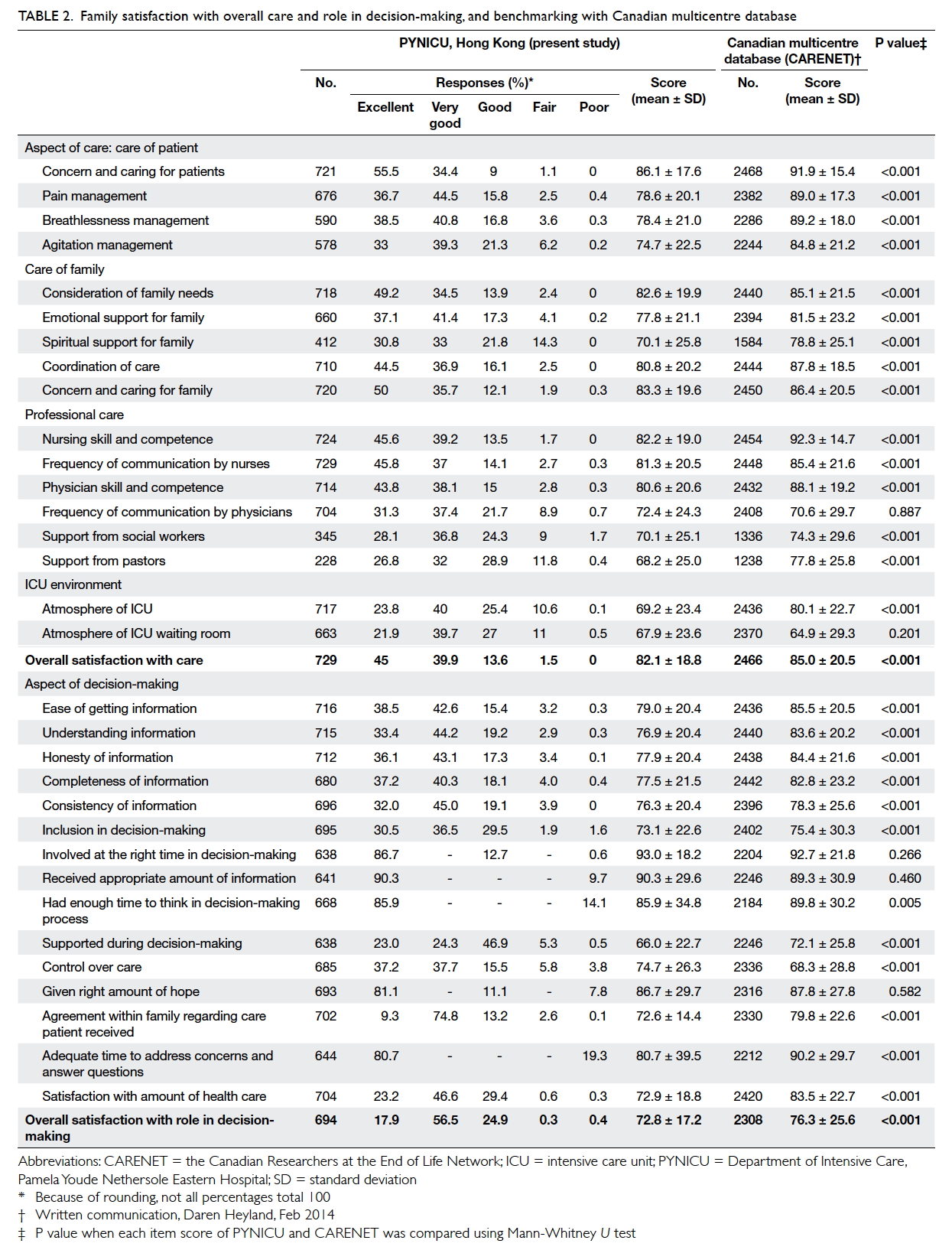
Table 2. Family satisfaction with overall care and role in decision-making, and benchmarking with Canadian multicentre database
When results were compared with the
Canadian data (written communication, Daren Heyland, Feb 2014), the latter had a higher mean FS-ICU/Total, FS-ICU/Care, and FS-ICU/DM score of 82.9
± 14.8, 83.5 ± 15.4, and 82.6 ± 16.0, respectively
(P<0.001 for all three scores when compared with
PYNICU). Table 2 shows the result for each FS-ICU item; PYNICU achieved a significantly higher
mean score for item “control over care”. There was
no significant difference in scores between the two
databases for items “frequency of communication by physicians”,
“atmosphere of ICU waiting room”, “involved at the
right time in decision-making”, “received appropriate
amount of information”, and “given right amount of
hope”. The Canadian sites achieved higher scores for
the remaining items.
In the univariate analysis of satisfaction
with overall ICU care, none of the patient’s or
respondent’s characteristics had a P≤0.1. Items
“spiritual support for family”, “support from social
workers”, and “support from pastors” were excluded
since more than 30% of the responses were either
missing or deemed not applicable. Thus, a total of
14 covariates were analysed in the multivariable
analysis. The independent factors identified
were “concern and caring for patients”, “agitation
management”, “concern and caring for family”,
“frequency of communication by nurses”, “physician skill and
competence”, “atmosphere of ICU”, and “atmosphere
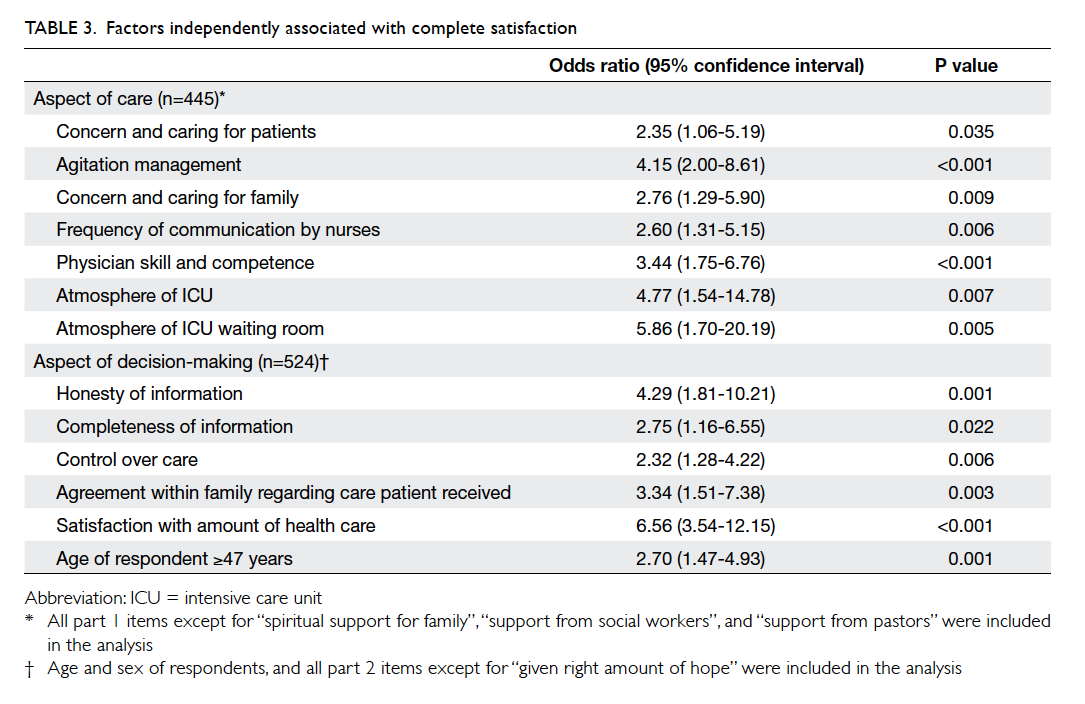
of ICU waiting room” (Table 3). In the multivariable analysis of satisfaction with role in decision-making,
16 covariates including “age of respondent”, “sex
of respondent” (with P values of 0.005 and 0.08,
respectively in the univariate analysis), and all items
in part two of the questionnaire excluding item
“given right amount of hope” (P=0.214 in univariate
analysis) were tested. Independent factors identified
were “honesty of information”, “completeness of
information”, “control over care”, “agreement within
family regarding care patient received”, “satisfaction
with amount of health care”, and “age of respondent
≥47 years” (Table 3).
Performance-importance plots identified
the following items as being more important but
performed less satisfactorily: “atmosphere of ICU
waiting room”, “atmosphere of ICU”, “agitation
management” (overall care), and “satisfaction
with amount of health care”
(decision-making) [Fig 1].
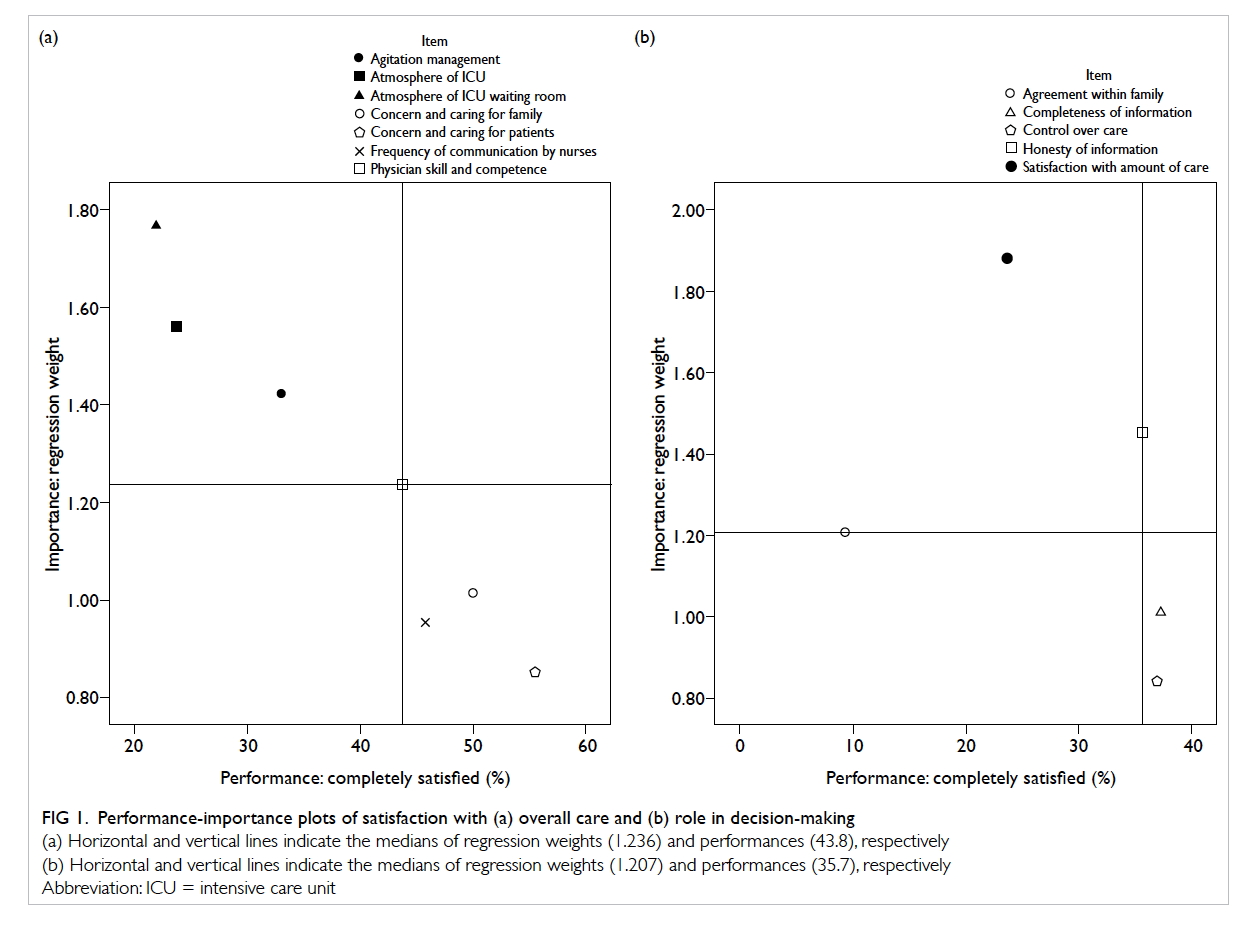
Figure 1. Performance-importance plots of satisfaction with (a) overall care and (b) role in decision-making
(a) Horizontal and vertical lines indicate the medians of regression weights (1.236) and performances (43.8), respectively
(b) Horizontal and vertical lines indicate the medians of regression weights (1.207) and performances (35.7), respectively
Discussion
This is the first ICU family satisfaction survey
published in Hong Kong, and was conducted
following implementation of the FAME programme
in 2012. Following a small-scale survey carried out by
PYNICU in 2010 (written communication, HL Wu,
2012), staff awareness about the importance of family
satisfaction has increased. Family satisfaction was
added to the regular agenda at our weekly business
meetings, where comments and feedback from NOKs
were discussed. These discussions led to various
measures to improve communication (unsolicited
nurses’ update during visiting hours), access to
information (information booklets in waiting rooms
and noticeboard displays for families), and facilities
(chairs for families at bedside, televisions for awake
patients, and refurbishment of the waiting rooms).
This survey showed high satisfaction scores in 2012 to
2014 that were similar to figures reported around the
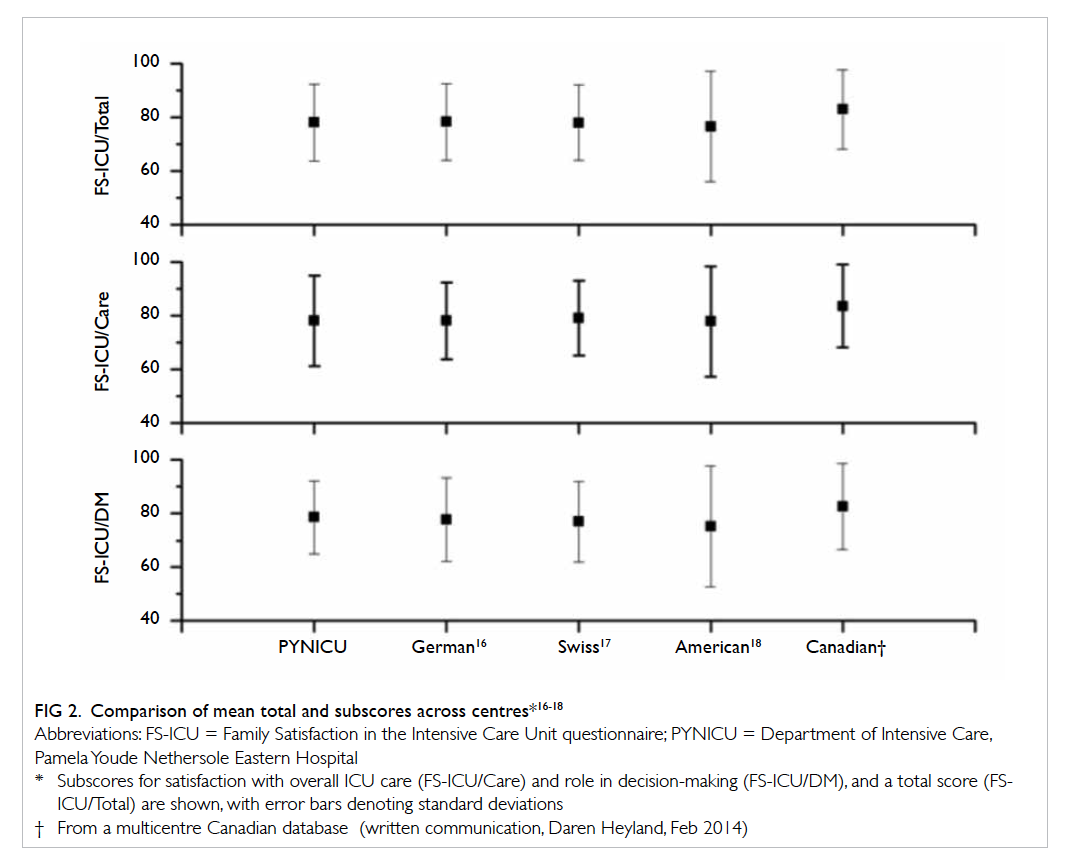
world (Fig 2 16 17 18 as well as the multicentre Canadian database—a German study reported their
mean FS-ICU/Total, FS-ICU/Care, and FS-ICU/DM
as 78.3 ± 14.3, 78.6 ± 14.3, and 77.8 ± 15.616; a Swiss
study reported scores of 78 ± 14, 79 ± 14, and 77 ±
1517; and an American study achieved scores of 76.6
± 20.6, 77.7 ± 20.6, and 75.2 ± 22.6, respectively.18
Nonetheless the Canadian centres were able to
achieve a significantly better result in most items and
in the summary scores. This might be explained by
cross-cultural (different expectations from families),
as well as administrative differences (nurse-patient
and doctor-patient ratios), but it may also indicate
room for further improvement.
Independent factors that affected satisfaction
with overall care and identified by this study can be
grouped into: care of the patient and family (concern
and caring for the patient and family; agitation
management), professional care (frequency of communication by nurses; physician skill and competence),
and the ICU environment (atmosphere of the ICU
and its waiting room). Consistent with prior studies,
none of the patient’s or respondent’s characteristics,
including the ICU survival status, was found to be
independently associated with satisfaction of overall
care.16 19 Setting professional skills aside, the perceived
physician competence and amount of concern and
care shown to patients and their families were largely
affected by the communication skill of the health
care providers and their manner when interacting
with patients and families. The importance of
communication has been emphasised by numerous
studies.20 21 22 23 24 25 One study found that longer periods of communication between health care providers and
families was associated with reduced anxiety among
family members of ICU patients.24 They reported
a median (range) time of staff contact as 10 (1-60)
minutes. In addition to the duration, a proactive,
structured, and multidisciplinary communication
strategy that incorporated the five objectives in
the mnemonic “VALUE” (to Value and appreciate
what the family members said, to Acknowledge the
family members’ emotions, to Listen, to ask open-ended
questions that would allow the caregiver to
Understand who the patient was as a person, and to
Elicit questions from family members) was shown to
lessen symptoms of anxiety, depression, and post-traumatic
stress disorder.25 Education and training
in communication skills, especially the power of
listening and to allow families more opportunity
to speak during conferences also improved family
satisfaction in the ICU.26 It is also essential to
diagnose the root cause of any communication
problem.15 Removing barriers in the health care
system that discourage communication, for example
heavy workload rendering insufficient time spent
with families and restrictive visiting policies, would
be beneficial.27
Factors in the left upper quadrant of the
performance-importance plots (Fig 1) had greater
regression weights but performed less satisfactorily,
and therefore warrant more urgent attention. Among
these were the ICU and waiting room environment.
The questionnaire items do not specify the particular
areas of concern that individual families had in mind,
but responses to the three open-ended questions
were illuminating. Comments related to the ICU
environment focused on the availability of facilities
for patients (visual and audio entertainment devices)
and their families (chairs and toilet), ICU noise level,
room temperature, space, and privacy. In fact, the
ICU environment has been repeatedly identified as a
factor that affects satisfaction.13 18 19 One study found that migration of an ICU with multiple beds in one
ward to another with single-room design significantly
improved family and patient satisfaction.13 These
findings offer opportunities for improvement, and
also provide valuable information for administrators
when designing a new ICU.
Agitation management also warranted more
urgent attention (Fig 1a). Although evidence
supports maintenance of a light rather than deep
level of sedation in adult critically ill patients to
shorten duration of mechanical ventilation and
ICU length of stay,28 29 a balance needs to be struck
to prevent excessive pain, agitation, or adverse
experiences that are associated with a higher
incidence of post-traumatic stress disorder in
ICU survivors and could negatively impact their
families.30 The revised 2013 version of Clinical
Practice Guidelines for the Management of Pain,
Agitation, and Delirium in Adult ICU Patients has
recommended routine monitoring of the depth of
sedation and targeted titration of preferably non-benzodiazepine
sedatives.31
Our subscore for decision-making was higher
than that for overall care, in contrast to the overseas
counterparts.16 17 18 We do not know if this is unique to the Chinese population since no other Chinese
survey is available for comparison. One interesting
finding was that younger respondents were less
satisfied with their role in decision-making than
older respondents. A similar observation has been
made before.32 In this information explosion era
where electronic data are easily available, it can be
understood that the younger generation wants to
play a greater role in making decisions for their sick
family member. A paternalistic approach will be less
appealing to our future generation, and a deliberative
model should therefore be adopted, with an emphasis
on provision of complete and honest information to
increase their sense of control over the care of their
family member.
There are limitations to our study. First, the
reason for refusal to participate in the survey was
not documented and therefore we cannot rule out
a response bias, where dissatisfied families might
have declined participation in the survey, thus
overestimating satisfaction. The high return rate
compared with other studies (76.6% vs 27.8-75.4%15 16 17)
would have lessened any effect of a response bias.
Second, social desirability bias cannot be ruled out
as most respondents completed the questionnaire
while their sick family member was still under
our care. We tried to minimise this by reassuring
families of the confidentiality of their response
and providing an envelope in which to return the
completed questionnaire that was only opened by
researchers at a later time. Third, questionnaires
completed before ICU discharge might not reflect
the whole ICU experience. Recruiting NOKs when
the patient was nearing ICU discharge reduced
premature data capture and prevented the otherwise
increased administrative cost, increased recall bias,
and anticipated lower response rate that would be
involved when tracing eligible NOKs following ICU
discharge. Fourth, FS-ICU has not been validated
in the Chinese language. The Chinese (Taiwan)
version provided by CARENET was modified by the
co-authors wherein Taiwanese terms were replaced
by ones familiar to the Hong Kong people and
questions on the respondent’s demographics were
added as in the original English questionnaire. This
modified version was circulated to and approved by
all co-authors to ensure face validity. The high return
rate of the questionnaire and the high response rate
to questions (95.0%) indicated feasibility of this
modified Chinese version.11 Last, this was a single-centre
study and thus generalisability of the results
to other settings may not be appropriate.
Conclusions
Family satisfaction is an important measure of ICU
quality. We found that families were satisfied with
the ICU care we provided and with their role in
decision-making. Their satisfaction was comparable
with most overseas centres. Nonetheless there
remains room for improvement when compared
with the Canadian database. Future initiatives will
focus on improving the ICU environment, agitation
management, and enhancing communication with
families.
Acknowledgements
We wish to thank all members of the FAME team
including Dr Arthur CW Lau, Ms Nora LP Kwok,
Ms L Lau, Ms CH Lee, and Ms HY Wong for their
administrative advice and contribution in data
collection and entry, and Ms CH Li, Ms WY So,
and Ms PS Chiu for subject recruitment. We also
wish to thank the Canadian Researchers at the End of
Life Network for sharing their FS-ICU database.
Current versions of the FS-ICU questionnaire can
be found on their website <www.thecarenet.ca/57-researchers/our-projects/family-satisfaction-survey>.
References
1. Davidson JE, Powers K, Hedayat KM, et al. Clinical
practice guidelines for support of the family in the patient-centered
intensive care unit: American College of Critical
Care Medicine Task Force 2004-2005. Crit Care Med
2007;35:605-22. Crossref
2. Lewin SA, Skea ZC, Entwistle V, Zwarenstein M, Dick J.
Interventions for providers to promote a patient-centred
approach in clinical consultations. Cochrane Database Syst
Rev 2001;(4):CD003267. Crossref
3. Roter DL, Hall JA, Kern DE, Barker LR, Cole KA, Roca
RP. Improving physicians’ interviewing skills and reducing
patients’ emotional distress. A randomized clinical trial.
Arch Intern Med 1995;155:1877-84. Crossref
4. Stewart M, Brown JB, Donner A, et al. The impact of patient-centered
care on outcomes. J Fam Pract 2000;49:796-804.
5. Heyland DK, Tranmer JE; Kingston General Hospital ICU
Research Working Group. Measuring family satisfaction
with care in the intensive care unit: the development
of a questionnaire and preliminary results. J Crit Care
2001;16:142-9. Crossref
6. Sundararajan K, Martin M, Rajagopala S, Chapman MJ.
Posttraumatic stress disorder in close relatives of intensive
care unit patients’ evaluation (PRICE) study. Aust Crit
Care 2014;27:183-7. Crossref
7. Schmidt M, Azoulay E. Having a loved one in the ICU: the
forgotten family. Curr Opin Crit Care 2012;18:540-7. Crossref
8. Davidson JE, Jones C, Bienvenu J. Family response to
critical illness: postintensive care syndrome-family. Crit
Care Med 2012;40:618-24. Crossref
9. Flaatten H. The present use of quality indicators in the
intensive care unit. Acta Anaesthesiol Scand 2012;56:1078-83. Crossref
10. de Vos M, Graafmans W, Keesman E, Westert G, van der
Voort PH. Quality measurement at intensive care units:
which indicators should we use? J Crit Care 2007;22:267-74. Crossref
11. Stricker KH, Niemann S, Bugnon S, Wurz J, Rohrer O,
Rothen HU. Family satisfaction in the intensive care unit:
cross-cultural adaptation of a questionnaire. J Crit Care
2007;22:204-11. Crossref
12. Wall RJ, Engelberg RA, Downey L, Heyland DK, Curtis
JR. Refinement, scoring, and validation of the family
satisfaction in the intensive care unit (FS-ICU) survey. Crit
Care Med 2007;35:271-9. Crossref
13. Jongerden IP, Slooter AJ, Peelen LM, et al. Effect of intensive
care environment on family and patient satisfaction: a
before-after study. Intensive Care Med 2013;39:1626-34. Crossref
14. Tastan S, Iyigun E, Ayhan H, Kilickaya O, Yilmaz AA,
Kurt E. Validity and reliability of Turkish version of family
satisfaction in the intensive care unit. Int J Nurs Pract
2014;20:320-6. Crossref
15. Heyland DK, Rocker GM, Dodek PM, et al. Family
satisfaction with care in the intensive care unit: results of a
multiple center study. Crit Care Med 2002;30:1413-8. Crossref
16. Schwarzkopf D, Behrend S, Skupin H, et al. Family
satisfaction in the intensive care unit: a quantitative and
qualitative analysis. Intensive Care Med 2013;39:1071-9. Crossref
17. Stricker KH, Kimberger O, Schmidlin K, Zwahlen M,
Mohr U, Rothen HU. Family satisfaction in the intensive
care unit: what makes the difference? Intensive Care Med
2009;35:2051-9. Crossref
18. Osborn TR, Curtis JR, Nielsen EL, Back AL, Shannon
SE, Engelberg RA. Identifying elements of ICU care
that families report as important but unsatisfactory:
decision-making, control, and ICU atmosphere. Chest
2012;142:1185-92. Crossref
19. Hunziker S, McHugh W, Sarnoff-Lee B, et al. Predictors
and correlates of dissatisfaction with intensive care. Crit
Care Med 2012;40:1554-61. Crossref
20. Scheunemann LP, McDevitt M, Carson SS, Hanson LC.
Randomized, controlled trials of interventions to improve
communication in intensive care: a systematic review.
Chest 2011;139:543-54. Crossref
21. Kodali S, Stametz RA, Bengier AC, Clarke DN, Layon AJ,
Darer JD. Family experience with intensive care unit care:
association of self-reported family conferences and family
satisfaction. J Crit Care 2014;29:641-4. Crossref
22. Lily CM, De Meo DL, Sonnar LA, et al. An intensive
communication intervention for the critically ill. Am J Med
2000;109:469-75. Crossref
23. Shelton W, Moore CD, Socaris S, Gao J, Dowling J.
The effect of a family support intervention on family
satisfaction, length-of-stay, and cost of care in the intensive
care unit. Crit Care Med 2010;38:1315-20. Crossref
24. Rusinova K, Kukal J, Simek J, Cerny V; DEPRESS
study working group. Limited family members/staff
communication in intensive care units in the Czech
and Slovak Republics considerably increases anxiety in
patients’ relatives—the DEPRESS study. BMC Psychiatry
2014;14:21. Crossref
25. Lautrette A, Darmon M, Megarbane B, et al. A
communication strategy and brochure for relatives of
patients dying in the ICU. N Engl J Med 2007;356:469-78. Crossref
26. McDonagh JR, Elliott TB, Engelberg RA, et al. Family
satisfaction with family conferences about end-of-life care
in the intensive care unit: increased proportion of family
speech is associated with increased satisfaction. Crit Care
Med 2004;32:1484-8. Crossref
27. Curtis JR, Patrick DL, Shannon SE, Treece PD, Engelberg
RA, Rubenfeld GD. The family conference as a focus to
improve communication about end-of-life care in the
intensive care unit: opportunities for improvement. Crit
Care Med 2001;29(2 Suppl):N26-33. Crossref
28. Kress JP, Pohlman AS, O’Connor MF, Hall JB. Daily
interruption of sedative infusions in critically ill patients
undergoing mechanical ventilation. N Engl J Med
2000;342:1471-7. Crossref
29. Girard TD, Kress JP, Fuchs BD, et al. Efficacy and safety
of a paired sedation and ventilator weaning protocol
for mechanically ventilated patients in intensive care
(Awakening and Breathing Controlled trial): a randomised
controlled trial. Lancet 2008;371:126-34. Crossref
30. Granja C, Gomes E, Amaro A, et al. Understanding
posttraumatic stress disorder–related symptoms after
critical care: the early illness amnesia hypothesis. Crit Care
Med 2008;36:2801-9. Crossref
31. Barr J, Fraser GL, Puntillo K, et al. Clinical practice
guidelines for the management of pain, agitation, and
delirium in adult patients in the intensive care unit. Crit
Care Med 2013;41:263-306. Crossref
32. Crow R, Gage H, Hampson S, et al. The measurement of
satisfaction with healthcare: implications for practice from
a systematic review of the literature. Health Technol Assess
2002;6:1-244. Crossref