Hong Kong Med J 2015 Aug;21(4):345–52 | Epub 19 Jun 2015
DOI: 10.12809/hkmj144399
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
REVIEW ARTICLE
Strategies and solutions to alleviate access block and overcrowding in emergency departments
Stewart SW Chan, MSc, FHKAM (Emergency Medicine);
NK Cheung, MB, ChB, FHKAM (Emergency Medicine);
Colin A Graham, MD, FCEM;
Timothy H Rainer, MD, FIFEM
Emergency Department, Prince of Wales Hospital; Accident and Emergency Medicine Academic Unit, The Chinese University of Hong Kong, Shatin, Hong Kong
Corresponding author: Dr Stewart SW Chan (stewart_chan@hotmail.com)
Abstract
Objectives: Access block refers to the delay caused
for patients in gaining access to in-patient beds after
being admitted. It is almost always associated with
emergency department overcrowding. This study
aimed to identify evidence-based strategies that can
be followed in emergency departments and hospital
settings to alleviate the problem of access block
and emergency department overcrowding; and to
explore the applicability of these solutions in Hong
Kong.
Data sources: A systematic literature review was
performed by searching the following databases:
CINAHL, Cochrane Database of Systematic Reviews,
EMBASE, MEDLINE (OVID), NHS Evidence,
Scopus, and PubMed.
Study selection: The search terms used were
“emergency department, access block, overcrowding”.
The inclusion criteria were full-text articles,
studies, economic evaluations, reviews, editorials,
and commentaries. The exclusion criteria were
studies not based in the emergency departments or
hospitals, and abstracts.
Data extraction: Abstracts of identified papers
were screened, and papers were selected if they
contained facts, data, or scientific evidence related
to interventions that aimed at improving outcome
measures for emergency department overcrowding
and/or access block. Papers identified were used to locate further references.
Data synthesis: All relevant scientific studies
were evaluated for strengths and weaknesses using
appraisal tools developed by the Critical Appraisal
Skills Programme. We identified solutions broadly classified into the following categories: (1)
strategies addressing emergency department
overcrowding: co-locating primary care within the
emergency department, and fast-track and emergency
nurse practitioners; and (2) strategies addressing
access block: holding units, early discharge and
patient flow, and political action—management and
resource priority.
Conclusion: Several evidence-based approaches
have been identified from the literature and effective
strategies to overcome the problem of access block
and overcrowding of emergency departments may
be formulated.
Introduction
In the past 20 years, access block and emergency
department (ED) overcrowding have emerged and
given rise to major problems, affecting the health
care systems of developed countries, including those
in the US, UK, and Australia.1 2 3 4 In Australia, the
term ‘access block’ is defined as the situation where
patients in EDs are unable to gain access to in-patient
beds within 8 hours of presentation to the ED.4 In
the UK, it is defined as 4 hours or more from arrival
to admission, transfer, or discharge.3 Although ED
overcrowding may be due to many factors other
than access block—such as increased ED attendances,
inappropriate use of ED services, or deficiencies in
ED medical and nursing staffing levels or patterns—access block is almost always associated with
overcrowding, and significantly leads to poor quality
of care outcomes.5 Numerous studies from the US,
UK, Canada, and Australia have shown that access
block causes ED overcrowding and affects quality
of care.6 7 8 9 10 Bullard et al8 reported that admitted patients “boarding” in the ED (ie access block) was
the number one advocacy issue for the Canadian
Association of Emergency Physicians. Richardson9
conducted a survey from 83 EDs in Australia and
concluded that overall, caring for patients waiting for
beds represented 40% of the workload of ED staff in
major hospitals. Apart from this, ED overcrowding
affects the outcomes of admitted patients. Sun et al10
performed a retrospective cohort analysis of 995 379
ED visits resulting in admissions in 187 acute care
hospitals in California, US, and found that periods
of ED overcrowding were associated with increased
mortality, longer length of stay, and higher costs for
admitted patients.
Access block and ED overcrowding are
detrimental to the morale of ED staff members.11
Moreover, a survey of 400 admitted ED patients by
Bartlett and Fatovich12 in Perth, Australia reported
that patients preferred waiting in ward corridors for a
ward bed if there were no ED cubicles available. This
study alone showed that access block, independent
of overcrowding, affects patients. Jelinek et al13 also
showed that overcrowding in the ED affects the
supervision of junior doctors.
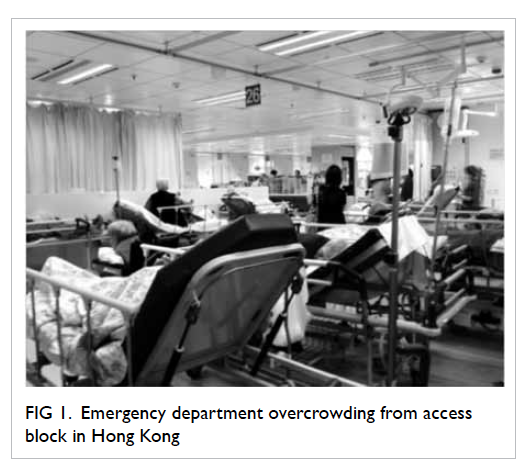
Overcrowding and access block in EDs are
rapidly becoming problematic areas for the health
system even in Hong Kong. Figure 1 shows a photograph depicting the crowded ED with literally
dozens of patients waiting for admission, which is
almost an everyday scenario in a major teaching
hospital in Hong Kong. At the time of drafting of
this manuscript, the hospital management had set a
target that patients waiting for admission should not
have to wait longer than 24 hours (Fig 2), a target that
is ludicrous by international standards. This review
therefore aimed to answer the question: what are
evidence-based strategies and solutions that can be
applied within the ED and the hospital setting that are
shown to be effective in alleviating ED overcrowding
and access block? Further, we explored the relevance
and applicability of these solutions identified with
respect to the Hong Kong setting.
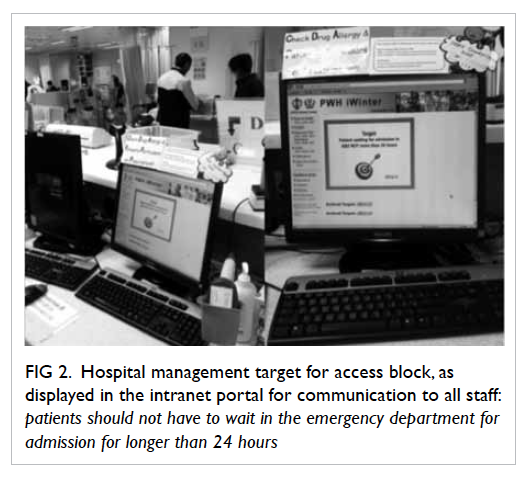
Figure 2. Hospital management target for access block, as displayed in the intranet portal for communication to all staff: patients should not have to wait in the emergency department for admission for longer than 24 hours
Methods
A search for English language papers was performed
on the following electronic databases: CINAHL,
Cochrane Database of Systematic Reviews, EMBASE,
MEDLINE (OVID), NHS Evidence, Scopus, and
PubMed. The search terms used were: “emergency
department, access block, overcrowding”. The
inclusion criteria were: full-text articles, randomised
controlled trials, systematic reviews, cohort studies,
case-control studies, qualitative studies, economic
evaluations, narrative reviews, editorials, and
commentaries. The exclusion criteria were studies
with interventions that were not primarily based in
the ED or hospital (eg primary care or pre-hospital
strategies) and abstracts.
Abstracts of identified papers were screened,
and papers were selected if they contained facts,
data, or scientific evidence related to interventions
that aimed at improving outcome measures for
ED overcrowding and/or access block. References
identified from these articles were used to locate
further references. All relevant scientific studies
were evaluated for strengths and weaknesses by
using appraisal tools developed by the Critical
Appraisal Skills Programme, which can be accessed
through the link: <http://www.casp-uk.net/>.
Results
The number of citations returned from the search
was as follows: CINAHL (11), Cochrane Database
of Systematic Reviews (0), EMBASE (39), MEDLINE
(OVID) [11], NHS Evidence (166), Scopus (32), and
PubMed (20). These citations were screened for
relevance and fulfilment of inclusion and exclusion
criteria. A total of 22 papers were selected which
included one systematic review, 12 cohort studies, seven
reviews, one qualitative study, and one expert opinion
article. From these article references, more papers
that were relevant to the subject were found and
studied.
The review identified numerous management
interventions that were likely to be effective in
improving outcome measures to prevent ED
overcrowding and access block. They are organised
and listed below:
(1) Strategies primarily addressing ED
overcrowding:
(a) Co-locating primary care within the ED; and
(b) Fast-track and emergency nurse practitioners (ENPs).
(a) Co-locating primary care within the ED; and
(b) Fast-track and emergency nurse practitioners (ENPs).
(2) Strategies primarily addressing access block:
(a) Holding units;
(b) Early discharge and patient flow; and
(c) Political action—management and resource priority.
(a) Holding units;
(b) Early discharge and patient flow; and
(c) Political action—management and resource priority.
Discussion
Strategies primarily addressing overcrowding in emergency departments
Co-locating primary care within the emergency departments
Overcrowding of ED has been attributed to primary
care attenders inappropriately utilising the ED.14 15
If this were true, then the provision for additional
number of primary care practitioners to the ED
physician workforce would follow as a possible
logical solution to counter ED overcrowding.
There is a wide variation in the incidence of
primary care attendance in the ED, with figures
ranging from 6% to 60% among hospitals in the UK.16
Variations in these studies may be due to differences
in concept as to what primary care problems need
or need not be treated in the ED.17 It was shown that
expanding primary care and out-of-hour services
may lead to decreased primary care attendance
at EDs.18 A considerable proportion of patients
attending the ED could be adequately looked after
by general practitioners (GPs) or primary care
physicians. Although it is considered cost-effective,
one study did find that GPs tend to utilise more
resources and another study showed that providing
primary care services in the ED actually increased
the number of primary care attendances, resulting in
increased waiting time.19 20 21
The synthesis of all these studies suggests that
co-locating primary care within the ED is a workable
solution in most instances, but the extent of the
benefits will depend on the relative importance of
primary care attendance as a cause for overcrowding,
which differs from country to country and from one
hospital to another. In Hong Kong, the principle
behind this solution has already been applied in
several hospitals, but is yet to be developed into a
territory-wide systematic strategy. In the past several
years, some hospitals have started to employ part-time
GPs to provide regular session-based services
in the ED. Their duty is to handle cases of low acuity and this has considerably helped in reducing
congestion at EDs. Although there have not been
any published data to show that these arrangements
improve waiting times in Hong Kong, our experience
is that these locum doctors do alleviate overcrowding
whenever they are present. In our hospital’s ED,
the GPs are encouraged to discuss difficult cases
with senior doctors in the EDs, who would advise
on treatment or disposition, or even take over the
patient for further management. In this way, quality
of care can be ensured. This approach seems to be
promising and a model that can be improved and
developed further. Based on the cited evidence,
this may have implications beyond just solving the
manpower number issue unto a more comprehensive
strategy and direction in health care planning.
Fast-track and emergency nurse practitioners
The concept of fast-track service stems from the fact
that most of the crowding in an ED may actually
involve low acuity patients like those with minor
injuries or minor illnesses. Therefore, fast-track
services for such patients may be an important
front-end operational strategy to relieve congestion.
If the fast-track services are efficiently designed and
provided by dedicated staff at a designated area in
the ED, we can expect improvement in flow and
elimination of wastes, which may result in shorter
overall waiting times. A review by Yoon et al,22
commissioned by the Canadian Health Technology
Assessment, concluded that fast-track systems in EDs
are efficient, cost-effective, safe, and satisfactory for
patients. Since 2002, the UK National Health Service
(NHS) has also encouraged the national use of fast-track systems under the ‘see and treat’ principle.3
The introduction of fast-track systems has been
investigated in a wide variety of clinical settings.23 24 25 26
These studies found that fast-track systems decreased
patient waiting times and shortened the overall
length of stay in EDs. The rate of patients “left without
being seen” was also reduced. Further, quality of
care was not compromised, as shown by data on
patient satisfaction, unscheduled reattendance, and
mortality rates. A key principle of using fast-track
systems is to have experienced and competent staff
designated to ‘see and treat’ the patients.
Studies also suggest that having ENPs
incorporated into these systems for seeing and
treating front-end strategies may further increase
efficiency in relieving overcrowding. Emergency
nurse practitioners have been increasingly used
in EDs in the UK since the 1990s.27 Carter and
Chochinov28 performed a systematic review of ENPs
working in the ED by looking at the key outcome
measures of waiting times, patient satisfaction,
quality of care, and cost-effectiveness. They found
that ENPs can reduce waits, lead to high patient
satisfaction, and provide quality of care equivalent
to a mid-grade resident doctor, although the costs
of resident doctors are higher. A recent Australian
study which included ENPs and physicians working
in an ED fast-track unit of a tertiary hospital showed
that while the quality of care was high in both
groups, patient satisfaction score was significantly
higher with the ENP group than with the physician
group.29
In Hong Kong, formal training of ENPs has
been developed only recently. This started when two
experienced emergency nurses from the authors’
institution were funded by a charitable foundation
to receive ENP training in the UK in 2006. They
subsequently started their ENP practice in June
2007 with a scope of practice focusing primarily
on minor injuries. In 2010, a university master’s
programme for advanced ENPs was first established
in Hong Kong to provide education and training
for emergency nurses. Currently in our ED, ENPs
are on roster for 5 days a week to ‘see and treat’
patients, numbering up to 20 patients per 8-hour
shift, with holistic responsibilities which include
performing minor procedures such as suturing in
conjunction with a vast array of nursing care services
for the patients they have seen. A retrospective study
from our department reported that ENP services
reduced waiting time and processing time without
compromising quality of care.30 The future training
and development of more ENPs into the workforce,
and their incorporation into an ED fast-track
service, are promising strategies for alleviating ED
overcrowding in Hong Kong.
Nevertheless, there are certain issues that are
still stumbling blocks. Currently, nurses in Hong
Kong are not legally allowed to prescribe medications
and issue sick leave certificates. Therefore, ENPs are
not completely independent although they carry a
good amount of clinical load. The ENPs also need
autonomy to refer patients for X-rays and allied
health services (eg physiotherapy) and these are
important barriers for effective development of their
service. Finally, there is a debate as to how cost-effective
it is to designate an ENP (at least at the grade
of Advanced Practising Nurse) to perform duties
that can be performed by a junior resident doctor.
The answer to this question will depend very much
on the relative supply of each of these categories of
staff prevailing at that point of time.
Strategies primarily addressing access block
The possible causes of access block include (1) the
disinclination for clinicians to discharge patients,
(2) inefficient flow in the discharge process, and (3)
genuinely insufficient bed capacity. These causes of
access block are discussed further and addressed
under the following three possible solutions.
Holding units
Holding units are clinical decision units or
observation units within the ED. In the US, reviews
by the Institute of Medicine Committee found that
such units were able to reduce the need for boarding
or ambulance diversion, which means these were
able to alleviate access block and ED overcrowding.31
They also contribute to reduction in hospitalisation
and improvements in ambulatory care. In 2007, 1746
EDs in the US reported having observation units
and this constituted about 36% of the total number
of EDs.32 Among them, 56% were administratively
managed by ED staff. In the UK, Cooke et al3 also
reviewed the use of observation units and found
that they might reduce length of stay in the ED and
possibly in the hospital too. Nevertheless, the review
concluded that results of the studies were variable and
confounded by methodological issues. Experience in
an ED in Spain in 2009 showed
that opening of a 16-bed holding unit in the ED of
a 900-bed teaching hospital led to improvement in
access block.33 Observation units have also been shown
to play a role in selected clinical conditions, like
acute exacerbation of heart failure, which is known
to be a very common cause for hospital admission.34
Another condition in which observation units can
be helpful is acute pyelonephritis.35 A retrospective
cohort study was performed reviewing 633 patients
with pyelonephritis before and after the opening
of the observation unit. The proportion of patients
admitted to hospital from the ED decreased
significantly from 36% to 26% after the opening of
the observation unit.35
The functions and setup of these holding
units may differ from one institution to another. If
the setup is more like a short-stay ward or even an
in-patient ward, then its favourable effect on access
block may be attributed simply and chiefly from an
increase in the number of beds, as opposed to the
streamlining of management. In Hong Kong, the idea
of an ED observation unit is not new and many EDs,
including ours, have been running observation units
for the past 15 to 20 years. The difference is that,
over the past 3 to 4 years, many observation units
have been expanded with increased number of beds
and broader case-mix, and renamed as ‘Emergency
Medicine Wards’. For example, in our ED, the
20-bed observation unit was expanded to a 40-bed
Emergency Medicine Ward with introduction of
formal care protocols and pathways for managing
conditions such as congestive heart failure,
chronic obstructive airway diseases, deep venous
thrombosis, cellulitis, and pyelonephritis. From
our experience, we are skeptical if the Emergency
Medicine Ward has contributed significantly in
alleviating access block or ED overcrowding. This
ward has provided extra beds and obviously alleviated
some of the bed access problems. Therefore, it just
means that the duty and workload are shifted to
the ED with a cost involved, which includes space
and human resources at the minimum. Within the
holding unit context, further contributions over and
above this would require adherence to management
protocols that have been proven to safely reduce length of
stay or hospitalisation rates.
In Canada, Schull et al36 retrospectively
evaluated the effect of ED clinical decision units
on overall ED patient flow, comparing outcomes
(including length of stay, admission rate, etc)
between seven EDs which had implemented clinical
decision units and nine control EDs without clinical
decision units. They concluded that the benefits of
clinical decision units were just marginal and that
the potentials for gains in efficiency were limited.
In summary, there is some evidence for the
role of holding units for alleviating access block
and overcrowding but this needs to be incorporated
together with carefully planned clinical management
protocols and adequate support staff.
Early discharge and patient flow
In a recent study based on ED presentations, inpatient
admission, and discharge data from 23
hospitals in Queensland, Australia, it was shown
that during the days when ‘discharge peak’ lags behind
the peak in in-patient admissions, hospitals exhibit
increased levels of occupancy, in-patient and ED
length of stay, and increased access block.37 38
Initiatives directed at early in-patient discharges
would effectively mitigate the problem of ED
overcrowding and access block.
Since access block increases the clinical risk of
patients who might be deprived of timely attention,
assessment and management by various specialty
medical teams, considering earlier discharge of low-risk,
almost fully recovered in-patients in order to
create bed capacity for the incoming sick patients
would be an important principle worth putting into
practice, and for clinicians and managers to balance
the risks and benefits. This involves researching and
refining prediction rules to categorise the levels of
risk of discharging in-patients earlier.2 39 This process
is described as ‘reverse triage’, and described by Kelen
et al39 as to select patients who can be discharged
safely with little risk of serious consequence, in the
event of disasters that demand increased hospital bed
capacity. In 2012, an anecdotal report was published
describing how this reverse triage system was put
to effective use in an unexpected event resulting
in a sudden demand for beds.40 Although initially
described for use during disasters, this system is also
considered suitable even for everyday hospital use to
ensure safe management of hospital capacity or to
reduce access block.2 39
There is some evidence from a systematic
review of nine studies which showed that involving
social workers to support discharge of elderly
patients was able to reduce the readmission rate
within 6 to 12 months without apparent increase in
mortality. However, the effect on length of hospital
stay was uncertain.41 Expanding social work services
may help to prevent re-attendance, overcrowding,
and access block.
Discharge lounges are areas in the hospital
for patients to wait until transport and other
administrative discharge arrangements are
completed. A study found that after the introduction
of such lounges, there can be substantial savings in
bed hours (early discharge and reduced length of
stay).42 However, further studies focusing more on
economic evaluations are needed. In hospital wards,
delay in discharges may also be associated with
attitudes of staff members who think that quicker
discharges would result in more admissions, and
hence increased workload. Incentives and reward
programmes to motivate in-patient staff members
to speed up the discharge process are therefore
important.
Some studies have shown that modelling
methods using patient flow systems or bed
management techniques may improve the flow of
patients by identifying bottlenecks and key factors
driving access block. For example, Martin et al43
found that the greatest source of delay in patient
flow was the waiting time from an admission request
for bed to the actual time of exit from the ED for
admission. Some researchers have developed a
mathematical model using the ED census to predict
crowding, daily surge and operational efficiency, the
basic pattern of the ED census comprising input,
throughput and output.44 King et al45 showed that
through the application of “lean thinking” and by
process mapping followed by identification of value
streams in the ED, they were able to significantly
improve waiting times and length of stay in EDs.
Strategies can also be focused on addressing demand
on in-patient beds by gathering predictable data on
daily or weekly peaks and valleys, and be able to
distribute admissions more smoothly and evenly
across the weeks.2 46
Political action—management and resource priority
One logical and clear solution for managing access
block is to increase bed capacity, increase the number
of acute beds and corresponding staff strength in
the hospitals. In reality, this is an issue of resource
availability and prioritising, a problem which the
hospital management constantly grapples with, in an
attempt to find the best balance. Therefore, health
care institutional funders need to be convinced
that ED overcrowding and access block are issues
of significant importance compared to other areas
of health care, in which resource distribution is
also needed. Ultimately, when all other solutions
fail simply because the root cause of the problem is
a system capacity matter, then effective responses
need to come from the institutional and system-wide
level to increase capacity. There are many
avenues and methods by which the attention of
the government and health authority can be drawn
to help focus on increasing the number of acute
hospital beds and thereby reducing access block.
Health care professionals can press for changes by
taking collective actions, organising information
campaigns, lobbying, drawing attention of the
press and media, negotiations, and even by public
demonstrations.
The review by Moskop et al2 presented an
anecdotal report of an information campaign
conducted by doctors in Canada that effectively
influenced changes in the government funding
policies.47 In April 2005, emergency physicians at
Vancouver General Hospital, frustrated by their
ongoing failure to persuade hospital administration
to address their access block crisis, gave selected
patients a statement expressing their “non-confidence
in the ability of the Vancouver General
Hospital ED to provide safe, timely, and appropriate
emergency medical care.”47 Emergency physicians
at other hospitals in Vancouver expressed similar
concerns publicly.47 As a result of this campaign, the
provincial Ministry of Health injected significant
funding to address the problem during that period.47
In order to relieve access block, governments
can also set targets and performance measures for
hospitals and the most well known among them is the
4-hour rule introduced by the UK NHS in 2004.48 By
this measure, 98% of ED patients are to be seen and
either admitted, discharged, or transferred within 4
hours from the time of triage. This makes hospital
administration take more responsibility for the
problem of access block, which becomes a ‘hospital-wide issue’ rather than purely an ED problem. As a
result, emergency care was prioritised, government
funding was increased, facilities were upgraded,
and more staff employed in order that hospital EDs
can achieve the target.48 Before implementation of
the 4-hour rule, as many as 23% of patients waited
longer than 4 hours in the ED, but the 2007 statistics
show that 97.7% patients were assessed, treated, and
discharged within 4 hours.48 49 In 2009 in Perth, the
Western Australian government also introduced a
similar 4-hour rule for hospitals, whereby initially
85% and eventually 98% of patients presenting
to the ED should be either discharged home or
admitted into hospital within 4 hours.50 A study was
performed by retrieving hospital and patient data
which looked at outcome measures like mortality
rates, access block, and overcrowding rates pre-
and post-introduction of the 4-hour rule.50 It was
found that reversal of overcrowding coincided with
significant improvements in mortality rate in three
tertiary hospitals in which the rule was introduced.50
Although targets are intended to improve the quality
of care, sometimes patient care can be compromised
in order to meet stringent time targets, as seen with
Mid Staffordshire NHS Trust in the UK which was
reported to have neglected clinical needs and safety
of patients in order to achieve time targets.48 In 2011,
the 4-hour target in England was replaced by other
clinical indicators.
Limitations
Due to differences in health systems, some of the
solutions discussed in the Hong Kong perspective
may be less practicable in other countries. For
example, in some countries the number of primary
care physicians from the public system available
to participate in ED work may be limited; and the
private practitioners may generally be less motivated
to provide part-time services.
Conclusion
Several possible strategies and management
approaches effective in dealing with the complex
problem of access block and ED overcrowding in
hospitals have been identified and discussed. Some
of these solutions have been developed for many
years and are supported by current evidence, while
others are promising, warranting more detailed
investigation. The strategy to co-locate primary
care in the ED is worth evaluating more, the extent
of the benefits being dependent on the relative
predominance of ‘primary care attendance’ as a
cause of ED overcrowding, and the availability of GPs
or other primary care providers in the workforce.
Further development of fast-track or minor injury
units, the use of ‘see and treat’ strategies, and further
training of more ENPs are also important directions
to take. Holding units have been quite extensively
studied and there is some evidence for their role,
although these need to be incorporated together with
well-planned management protocols and adequate
staff support. ‘Reverse triage’ is a relatively new
concept and needs to be well formulated. Prediction
rules to select patients who can be discharged safely
with little risk of serious consequences have been
derived and can be used in the event of vast surges
in demand for hospital bed capacity. This may be
applicable for accelerating discharge of patients
safely in times of access block.
References
1. Moskop JC, Sklar DP, Geiderman JM, Schears RM,
Bookman KJ. Emergency department crowding, part 1—concepts, causes, and moral consequences. Ann Emerg
Med 2009;53:605-11. Crossref
2. Moskop JC, Sklar DP, Geiderman JM, Schears RM,
Bookman KJ. Emergency department crowding, part 2—barriers to reform and strategies to overcome them. Ann
Emerg Med 2009;53:612-7. Crossref
3. Cooke M, Fisher J, Dale J, et al. Reducing attendances and
waits in emergency departments. A systematic review of
present innovations. London: The National Coordinating
Centre for the Service Delivery and Organisation, London
School of Hygiene and Tropical Medicine; 2004.
4. Forero R, McCarthy S, Hillman K. Access block and
emergency department overcrowding. Available from:
http://ccforum.com/content/15/2/216. Accessed 1 Feb
2013.
5. Dunn R. Reduced access block causes shorter emergency
department waiting times: An historical control
observational study. Emerg Med 2003;15:232-8. Crossref
6. Forero R, Hillman KM, McCarthy S, Fatovich DM, Joseph
AP, Richardson DB. Access block and ED overcrowding.
Emerg Med Australas 2010;22:119-35. Crossref
7. Gilligan P, Winder S, Ramphul N, O’Kelly P. The referral
and complete evaluation time study. Eur J Emerg Med
2010;17:349-53. Crossref
8. Bullard MJ, Villa-Roel C, Bond K, Vester M, Holroyd B,
Rowe B. Tracking emergency department overcrowding in
a tertiary care academic institution. Healthc Q 2009;12:99-106. Crossref
9. Richardson D. 2008 – 2. Access block point prevalence
survey. The Australasian College for Emergency
Medicine 2008. Available from: https://www.acem.org.au/getattachment/e6442562-06f7-4629-b7f9-8102236c8b9d/Access-Block-2009-point-prevalence-study.aspx. Accessed
1 Feb 2013.
10. Sun BC, Hsia RY, Weiss RE, et al. Effect of emergency
department crowding on outcomes of admitted patients.
Ann Emerg Med 2013;61:605-11.e6. Crossref
11. Kilcoyne M, Dowling M. Working in an overcrowded
accident and emergency department: nurses’ narratives.
Aust J Adv Nurs 2007;25:21-7.
12. Bartlett S, Fatovich D. Emergency department patient
preferences for waiting for a bed. Emerg Med Australas
2009;21:25-30. Crossref
13. Jelinek GA, Weiland TJ, Mackinlay C. Supervision and
feedback for junior medical staff in Australian emergency
departments: findings from the emergency medicine
capacity assessment study. BMC Med Educ 2010;10:74. Crossref
14. Rajpar SF, Smith MA, Cooke MW. Study of choice between
accident and emergency departments and general practice
centres for out of hours primary care problems. J Accid
Emerg Med 2000;17:18-21. Crossref
15. Bianco A, Pileggi C, Angelillo IF. Non-urgent visits to a
hospital emergency department in Italy. Public Health
2003;117:250-5. Crossref
16. Murphy AW. ‘Inappropriate’ attenders at accident and
emergency departments I: definition, incidence and
reasons for attendance. Fam Pract 1998;15:23-32. Crossref
17. Gill JM, Reese CL 4th, Diamond JJ. Disagreement among
health care professionals about the care needs of emergency
department patients. Ann Emerg Med 1996;28:474-9. Crossref
18. Roberts E, Mays N. Accident and emergency care at
the primary-secondary interface: a systematic review
of the evidence on substitution. London: King’s Fund
Commission; 1997.
19. Dale J, Lang H, Roberts JA, Green J, Glucksman E.
Cost effectiveness of treating primary care patients in
accident and emergency: a comparison between general
practitioners, senior house officers, and registrars. BMJ
1996;312:1340-4. Crossref
20. Gibney D, Murphy AW, Smith M, Bury G, Plunkett PK.
Attitudes of Dublin accident and emergency department
doctors and nurses towards the services offered by local
general practitioners. J Accid Emerg Med 1995;12:262-5. Crossref
21. Krakau I, Hassler E. Provision for clinic patients in the ED
produces more nonemergency visits. Am J Emerg Med
1999;17:18-20. Crossref
22. Yoon P, Steiner I, Reinhardt G. Analysis of factors
influencing length of stay in the emergency department.
CJEM 2003;5:155-61.
23. Sanchez M, Smally AJ, Grant RJ, Jacobs LM. Effects of a
fast-track area on emergency department performance. J
Emerg Med 2006;31:117-20. Crossref
24. Rodi SW, Grau MV, Orsini CM. Evaluation of a fast
track unit: alignment of resources and demand results
in improved satisfaction and decreased length of stay for
emergency department patients. Qual Manag Health Care
2006;15:163-70. Crossref
25. O’Brien GM, Shapiro MJ, Woolard RW, O’Sullivan PS,
Stein MD. “Inappropriate” emergency department use:
a comparison of three methodologies for identification.
Acad Emerg Med 1996;3:252-7. Crossref
26. Kwa P, Blake D. Fast track: has it changed patient care in the
emergency department? Emerg Med Australas 2008;20:10-5. Crossref
27. Neades BL. Expanding the role of the nurse in the Accident
and Emergency department. Postgrad Med J 1997;73:17-22. Crossref
28. Carter AJ, Chochinov AH. A systematic review of the
impact of nurse practitioners on cost, quality of care,
satisfaction and wait times in the emergency department.
CJEM 2007;9:286-95.
29. Dinh M, Walker A, Parameswaran A, Enright N. Evaluating
the quality of care delivered by an emergency department
fast track unit with both nurse practitioners and doctors.
Australas Emerg Nurs J 2012;15:188-94. Crossref
30. Chung J, Way R, Rainer TH. Development of an emergency
nurse practitioner service in Hong Kong through
international collaboration: evaluation of the service
development. 1st Global Conference on Emergency
and Trauma Care; 2014 Sep 18-21; Dublin, Ireland. Int
Emerg Nurs 2014;22:237-60. Available from: http://www.internationalemergencynursing.com/article/S1755-599X(14)00280-8/fulltext. Accessed 6 Nov 2014.
31. Institute of Medicine Committee on the Future of
Emergency Care in the United States Health System.
Hospital-based emergency care: At the Breaking Point
(2007). Washington, DC: National Academies Press; 2006.
Available from: http://www.nap.edu/catalog/11621.html. Accessed 15 Feb 2013.
32. Wiler JL, Ross MA, Ginde AA. National study of
emergency department observation services. Acad Emerg
Med 2011;18:959-65. Crossref
33. Gómez-Vaquero C, Soler AS, Pastor AJ, Mas JR, Rodriguez
JJ, Virós XC. Efficacy of a holding unit to reduce access block
and attendance pressure in the emergency department.
Emerg Med J 2009;26:571-2. Crossref
34. Collins SP, Schauer DP, Gupta A, Brunner H, Storrow AB,
Eckman MH. Cost-effectiveness analysis of ED decision
making in patients with non-high-risk heart failure. Am J
Emerg Med 2009;27:293-302. Crossref
35. Schrock JW, Reznikova S, Weller S. The effect of an
observation unit on the rate of ED admission and discharge
for pyelonephritis. Am J Emerg Med 2010;28:682-8. Crossref
36. Schull MJ, Vermeulen MJ, Stukel TA, et al. Evaluating the
effect of clinical decision units on patient flow in seven
Canadian emergency departments. Acad Emerg Med
2012;19:828-36. Crossref
37. Khana S, Boyle J, Good N, Lind J. Early discharge and its
effect on ED length of stay and access block. In: Meader
AJ, Matin-sanchez FJ, editors. Health informatics:
building a healthcare future through trusted information.
Amsterdam: IOS Press; 2012: 92-8.
38. Khana S, Boyle J, Good N, Lind J. Unravelling relationships:
Hospital occupancy levels, discharge timing and
emergency department access block. Emerg Med Australas
2012;24:510-7. Crossref
39. Kelen GD, Kraus CK, McCarthy ML, et al. Inpatient
disposition classification for the creation of hospital surge
capacity: a multiphase study. Lancet 2006;368:1984-90. Crossref
40. Satterthwaite PS, Atkinson CJ. Using ‘reverse triage’ to
create hospital surge capacity: Royal Darwin Hospital’s
response to the Ashmore Reef disaster. Emerg Med J
2012;29:160-2. Crossref
41. Hyde CJ, Robert IE, Sinclair AJ. The effects of supporting
discharge from hospital to home in older people. Age
Ageing 2000;29:271-9. Crossref
42. Cowdell F, Lees B, Wade M. Discharge planning. Armchair
fan. Health Serv J 2002;112:28-9.
43. Martin M, Champion R, Kinsman L, Masman K.
Mapping patient flow in a regional Australian emergency
department: a model driven approach. Int Emerg Nurs
2011;19:75-85. Crossref
44. Flottemesch TJ, Gordon BD, Jones SS. Advanced statistics:
developing a formal model of emergency department
census and defining operational efficiency. Acad Emerg
Med 2007;14:799-809. Crossref
45. King DL, Ben-Tovim DI, Bassham J. Redesigning emergency
department patient flows: application of Lean Thinking to
health care. Emerg Med Australas 2006;18:391-7. Crossref
46. Litvak E, Buerhaus PI, Davidoff F, Long MC, McManus
ML, Berwick DM. Managing unnecessary variability in
patient demand to reduce nursing stress and improve
patient safety. Jt Comm J Qual Patient Saf 2005;31:330-8.
47. Abu-Laban RB. The junkyard dogs find their teeth:
addressing the crisis of admitted patients in Canadian
emergency departments. CJEM 2006;8:388-91.
48. Letham K, Gray A. The four-hour target in the NHS
emergency departments: a critical comment. Emergencias
2012;24:69-72.
49. Department of Health (UK). Hospital waiting times
and waiting lists. 2010. Available from: http://webarchive.nationalarchives.gov.uk/20100406182906/http://www.dh.gov.uk/en/Publicationsandstatistics/Statistics/Performancedataandstatistics/HospitalWaitingTimesandListStatistics/index.htm. Accessed 1 Mar 2013.
50. Geelhoed GC, de Klerk NH. Emergency department
overcrowding, mortality and the 4-hour rule in Western
Australia. Med J Aust 2012;196:122-6. Crossref