Hong Kong Med J 2015 Jun;21(3):261–8 | Epub 22 May 2015
DOI: 10.12809/hkmj144307
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
MEDICAL PRACTICE
Translating evidence into practice: Hong Kong Reference Framework for Preventive Care for
Children in Primary Care Settings
Natalie PY Siu, MB, BS, FHKAM (Family Medicine)1;
LC Too, MB, BS, FHKAM (Family Medicine)1;
Caroline SH Tsang, MB, ChB, FHKAM (Community Medicine)1;
Betty WY Young, MB, BS, FHKAM (Paediatrics)2;
1 Primary Care Office, Department of Health, Hong Kong
2 Clinical Advisory Group on Hong Kong Reference Framework for
Preventive Care for Children in Primary Care Settings, Hong Kong
Corresponding author: Dr Caroline SH Tsang (caroline_tsang@dh.gov.hk)
Abstract
There is increasing evidence that supports the close
relationship between childhood and adult health.
Fostering healthy growth and development of
children deserves attention and effort. The Reference
Framework for Preventive Care for Children in
Primary Care Settings has been published by the Task
Force on Conceptual Model and Preventive Protocols
under the direction of the Working Group on Primary
Care. It aims to promote health and prevent disease
in children and is based on the latest research, and
contributions of the Clinical Advisory Group that
comprises primary care physicians, paediatricians,
allied health professionals, and patient groups. This
article highlights the comprehensive, continuing,
and patient-centred preventive care for children
and discusses how primary care physicians can
incorporate the evidence-based recommendations
into clinical practice. It is anticipated that the
adoption of this framework will contribute to
improved health and wellbeing of children.
Introduction
Advances in socio-economic conditions and health
care delivery have contributed to improvement in
child health indices in Hong Kong. For example, the
infant mortality rate in Hong Kong is low by world
standards, decreasing from 9.7 per 1000 live births
in 1981 to 1.5 in 2012. Various problems, however,
continue to affect the health of Hong Kong children.
For instance, the increasing trend of obesity among
primary and secondary school children has become
a major public health concern.1 Injury is also a
significant cause of mortality and morbidity in
children. Many of these problems can be prevented.
In order to adopt the life-course approach to
chronic disease prevention and health promotion,
the Task Force on Conceptual Model and Preventive
Protocols under the Working Group on Primary Care
has identified two age-group–specific preventive
reference frameworks, one of which is the Reference
Framework for Preventive Care for Children in
Primary Care Settings.2 It was developed according to
the latest research evidence and with the support of
the Clinical Advisory Group that comprises primary
care physicians, specialists such as paediatricians,
allied health professionals, and patient groups.
Many medical professionals have difficulty
assimilating rapidly evolving scientific evidence into
their practice. The reference framework provides an
interface between research and practice, and aims
to support health care professionals to promote
health and provide continuing and comprehensive
care for children in the community. It consists of a
core document supplemented by a series of modules
that elaborate on the various domains relevant to
child health. This article highlights a practical use
of this reference framework to improve the delivery
of preventive care to children in the primary care
setting.
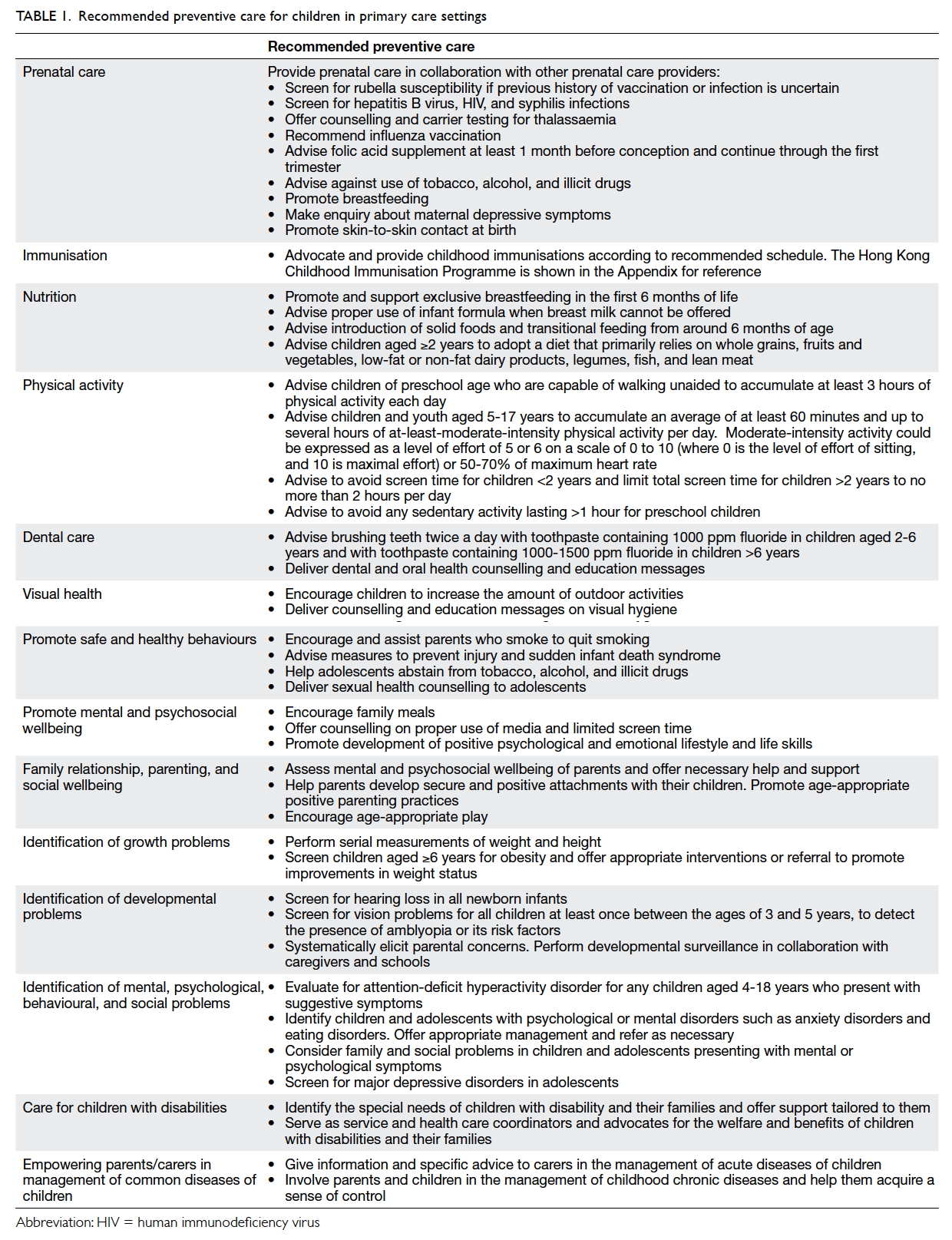
Evidence-based preventive care for children
The core document of the reference framework
provides evidence-based recommendations for
comprehensive preventive care for children and
can be categorised into various health domains,
ranging from prenatal care to care for children
with special needs. Preventive care activities for
children applicable to the primary care setting are
summarised in Table 1.
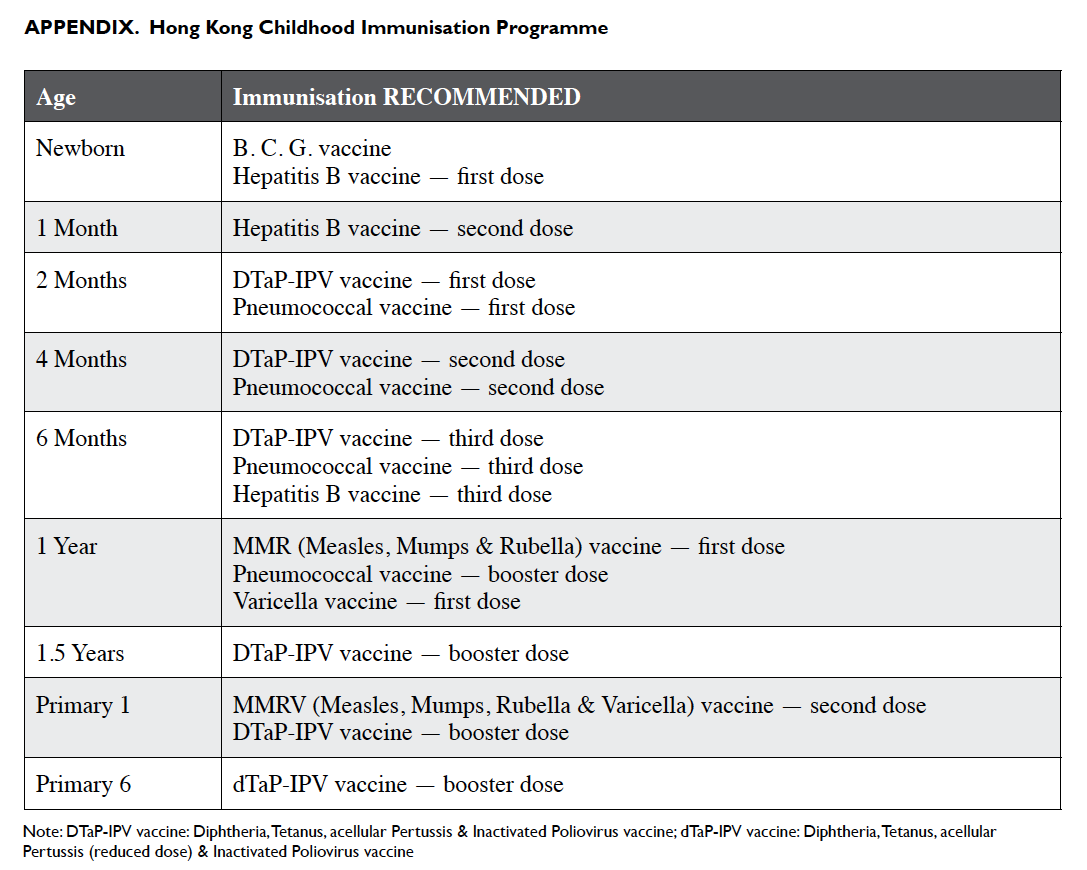
Continuing and patient-centred preventive care for children
The commitment of primary care physicians to
preventive care of children is vital in the prevention
of disease as well as early detection of problems
and appropriate intervention. Every encounter with
a child and/or the parents/caregivers should be an
opportunity to promote healthy practices. Some
forms of prevention should be delivered regularly,
for example, vaccinations that should adhere to the
locally recommended schedule. Other preventive
care may be offered opportunistically, such as advice
on dental care and physical activity. It is neither
possible nor appropriate to initiate all preventive
care at a single clinic visit. Nevertheless the long-term
relationship between primary care physicians
and patients allows provision of comprehensive and
continuing care.
Practising preventive care for children in primary care
Primary care physicians may not have adequate
time to go through the reference framework,
especially in a busy clinic setting. It is nonetheless
necessary to establish how recommendations of the
reference framework can be applied to patient care.
Four practical tips on application of the reference
framework will be discussed below.
Make use of the two-page summary
The Primary Care Office has developed a two-page
summary that can be downloaded from its
website (Fig 1). Tabulating the various preventive
activities according to age-group will enable primary
care physicians to provide suitable age-specific
preventive measures for their patients. The relevant
chapter of the core document is identified for each
aspect of preventive care, informing the primary
care physician of where to find further information
and supporting evidence. A summary can be posted
on walls or on the desk in primary care consultation
rooms to allow quick reference.
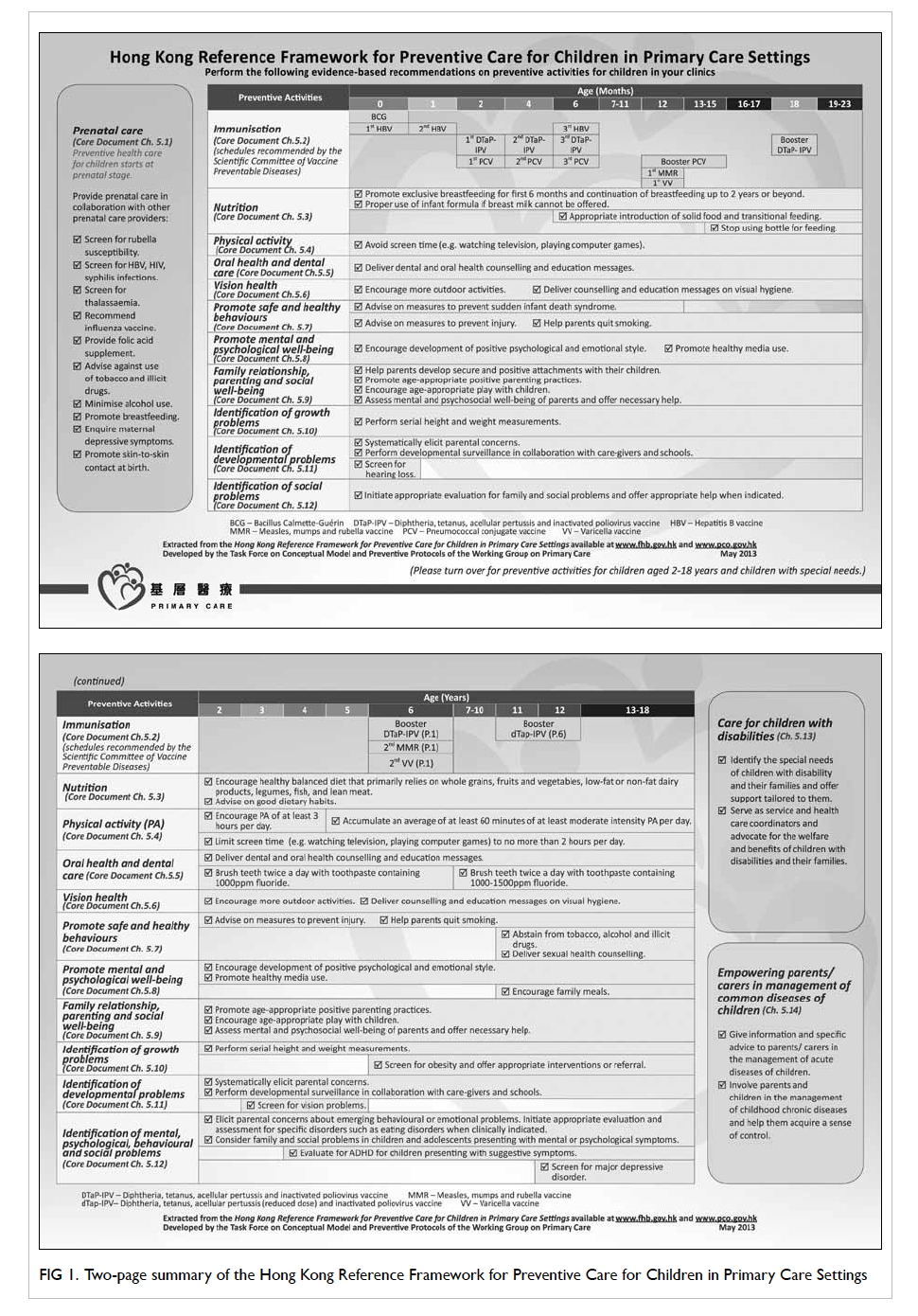
Figure 1. Two-page summary of the Hong Kong Reference Framework for Preventive Care for Children in Primary Care Settings
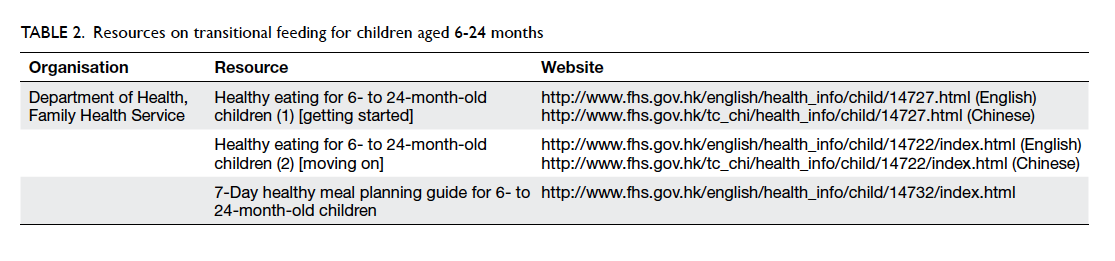
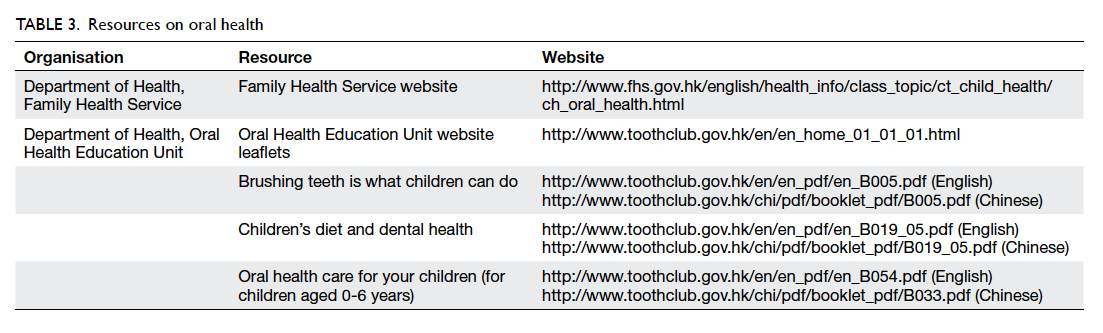
Make use of patient-education materials
Patient-based education interventions, especially
those that involve patient-education material, have
been reported to be effective in the implementation
of clinical practice guidelines.3 Patient-education
materials can also help more effectively deliver
preventive advice. Resources related to the health
care of children, such as transitional feeding (Table
2) and oral health (Table 3), are listed in annex 3 of
the core document. A link to these resources can
be accessed from the electronic version of the core
document. These can be introduced to children and
parents and enhance patient education.
Record preventive care activities using checklists
Embedding guideline evidence into the processes
and documents of patient care can help promote
established evidence-based recommendations.4
Checklists of opportunistic preventive care can
also be incorporated in patient medical records to
allow clear documentation and facilitate any follow-up
care. Primary care physicians can prepare their
own checklists or utilise the ready-made checklists
available in chapter 8 of the Module on Immunisation
(Fig 2).
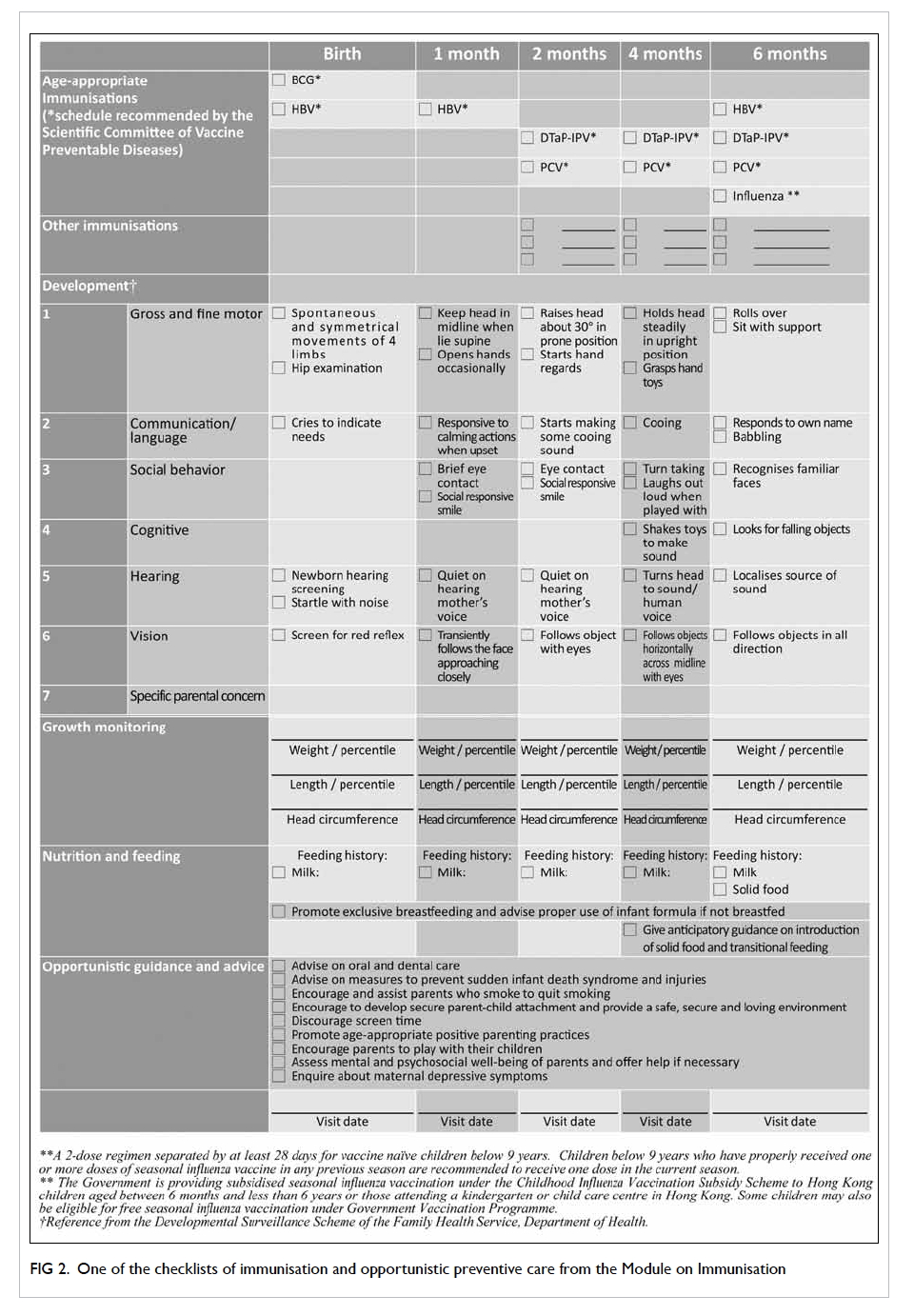
Figure 2. One of the checklists of immunisation and opportunistic preventive care from the Module on Immunisation
Deliver preventive care according to life stage
Childhood can be considered a sequence of life stages,
namely prenatal, infancy, preschool, school age, and
adolescence. Among the recommendations in Table 1, some items have particular relevance to particular
life stages. For the care of an individual child in the
primary care setting, preventive activities should be
appropriate for age, risk status, and individual needs
and values. Chapter 6 of the core document contains
tables of preventive care for different life stages, and
specifies the timing and action of various activities.
Such a tailored approach to recommendations may
ensure that the research-based message is more
easily translated.5 The practice of preventive care for
different life stages in daily practice can be illustrated
as follows.
Prenatal care
Prenatal care is essential for a healthy outcome of
pregnancy and should commence prior to conception.
All women planning pregnancy should take
daily folic acid supplement at a dose of 400 µg/day
for at least 1 month before conception, and continue
through the first trimester to reduce the risk of
having a baby with neural tube defect.6 7 If the
history of vaccination or infection is uncertain, the
woman should be screened for rubella susceptibility
and, if indicated, rubella vaccine administered 3
months before conception. Influenza vaccination
should also be offered.8 In addition, screening for
hepatitis B virus, human immunodeficiency virus,
and syphilis infections should be offered if it has not
been performed.9 10 11
Due to their harmful effect on fetal growth and
development, women should be questioned about
tobacco and alcohol use, and appropriate counselling
offered.12 13 Breastfeeding should be promoted
with relevant education and support commencing
prenatally.14 15
Infancy (0-24 months of age)
Children and families experience rapid changes
during the period of infancy. Immunisation for
various infectious diseases is vital at this stage. Each
visit of a child to their primary care physician provides
an opportunity to confirm that immunisations are up
to date. Other advice on preventive care can also be
given at the same time, such as promotion of breastfeeding. Primary care providers can refer to the core
document for strategies to promote breastfeeding
and the principles of transitional feeding.
The long-term relationship between primary
care physicians and families allows for surveillance
of a child’s growth and development. Serial
measurements of the weight and length of an infant
should be recorded on a population-specific growth
chart. Routine screening for hearing loss should also
be arranged.
Visits to the primary care physician’s clinic
provide an opportunity to observe relationships
between parents and their children. Secure
parent-child attachment in early childhood can be
protective and provide a foundation for exploration
and normal development.16 Parents can be helped to
understand the concept of attachment and develop
appropriate responses to the attachment behaviours
of their young children. Parents’ psychosocial wellbeing
and parenting capacity should be monitored
and assistance given when indicated.
Preschool (2-5 years of age)
Young children should be provided with a balanced
diet that comprises grains and cereals, vegetables
and meat (including its alternatives, eg fish, poultry,
eggs, beans, etc) in a ratio of 3:2:1 by volume.17
Ongoing surveillance of growth, and
physical and psychosocial development should
be undertaken in partnership with parents.
Screening for vision problems should be offered
for all children aged between 3 and 5 years to
detect amblyopia or the presence of any risk for its
development. Any parental concerns about a child’s
development such as hearing, language, gross and
fine motor development, and social behaviours
should be elicited systematically. Updating a child’s
developmental history by direct questioning of a
parent or carer can assist in the identification of any
abnormalities that warrant further investigation.
Parents should also be asked if they have any concerns
about their child’s behaviour. Testing for attention-deficit/hyperactivity disorder should be initiated if
academic or behavioural problems and symptoms of
inattention, hyperactivity, or impulsivity are present.
Parenting programmes have been shown to
improve both child behaviour and parenting.18 19 20 21 22 As such, they should be promoted to parents.
Toddlers are prone to injury as they are active
and love to explore their environment. Parents can be
given advice on how to maintain a safe environment
and prevent accidental injury.23
School age (6-12 years of age)
As children grow up, they can be expected to take
on additional responsibility for their health. Healthy
lifestyle advice, such as eating a healthy balanced
diet and taking adequate physical activity, can be
discussed during clinical consultations for episodic
illnesses. It is recommended that children aged 5
years and above be involved in at least 60 minutes
of moderate-to-vigorous–intensity physical activity
each day.24 25 26 Children should minimise sedentary
activity and avoid screen time of more than 2 hours
per day.27 28 29 Differences can be observed in physical
growth among children in this life stage. Screening
for obesity can be offered for children aged 6 years
and older, and appropriate weight maintained by
counselling and behavioural intervention where
indicated.30
School age is the time when learning difficulties
or behavioural problems start to manifest. Primary
care physicians can ask parents about progress at
school and academic performance. Poor school
performance may indicate an underlying learning or
attention disorder. Children should be referred for
detailed assessment if specific learning disabilities
are suspected.
Adolescence (13-18 years of age)
Adolescence is the key transition stage between
childhood and adulthood, a stage of attaining physical
and sexual maturity. Adolescents are curious about
new things and can be subject to peer pressure with
consequent engagement in risk behaviour. When
primary care physicians encounter adolescents, they
have an opportunity to explore their psychosocial
wellbeing. Information can be obtained about
social life and extracurricular activities. Healthy
activities such as sports and outdoor activities and
healthy use of the mass media can be promoted as
appropriate. If adolescents express boredom and loss
of interest in their usual activities, depression should
be suspected. Screening for a major depressive
disorder can be conducted when systems are in
place to ensure accurate diagnosis, psychotherapy,
and follow-up.31
Smoking status for all teenagers should be
established whenever the opportunity arises. Use
of alcohol and illicit drugs should also be assessed
using a non-judgemental approach. Adolescents
who abuse either should be assisted to quit and
referred for further management.32 33 Sexual history can be obtained and preventive counselling on
sexual health issues delivered.34 High-intensity
behavioural counselling is recommended to prevent
sexually transmitted infections in all sexually active
adolescents considered to be at increased risk.
Adolescents and their families should be
encouraged to eat together: frequency of family
meals has been inversely associated with poor
academic performance, depressive symptoms, and
risky behaviour such as tobacco and alcohol use.35
Conclusion
Chronic disease prevention and health promotion
can begin in childhood. Effective delivery of
preventive care to children depends on the
combined efforts of health care professionals, social
workers, teachers, and parents. Through provision
of patient-centred, comprehensive, continuing and
coordinated care, primary care physicians play
a vital role in preventive care for children. The
reference framework provides a common reference
and guidance on a spectrum of preventive care
activities for children. Adoption of the reference
framework, its accompanying two-page summary,
patient-education materials, and preventive care
checklist enhances delivery of care. Practice of
age-appropriate preventive care in different life
stages can improve the health and wellbeing of
children. Primary care physicians are in a privileged
position to incorporate recommendations of the
reference framework into clinical practice, and they
are encouraged to familiarise themselves with the
content of the reference framework. Development of
new modules is underway to provide practical tips
and information about topical issues already featured
in the core document of the reference framework.
Health care professionals are encouraged to visit
the website of the Primary Care Office at www.pco.gov.hk and watch out for the new modules to
be released, as well as information about seminars
related to introduction of the reference frameworks.
Feedback about implementation of the framework is
welcome and will be valuable for revision of the core
document and development of future modules.
References
1. Student Health Service. Newsletter [Internet]. December
2012; 57. Hong Kong SAR: Department of Health.
Available from: http://www.studenthealth.gov.hk/english/newsletters/newsletter_57.html. Accessed 18 Mar 2015.
2. Hong Kong reference framework for preventive care
for children in primary care settings 2012. Available
from: http://www.pco.gov.hk/english/resource/files/ref_framework_children.pdf. Accessed 13 Nov 2014.
3. Davis DA, Taylor-Vaisey A. Translating guidelines into
practice. A systematic review of theoretic concepts,
practical experience and research evidence in the adoption
of clinical practice guidelines. CMAJ 1997;157:408-16.
4. Gerhardt WE, Schoettker PJ, Donovan EF, Kotagal UR,
Muething SE. Putting evidence-based clinical practice
guidelines into practice: an academic pediatric center’s
experience. Jt Comm J Qual Patient Saf 2007;33:226-35.
5. Yana R, Jo RM. Getting guidelines into practice: a literature
review. Nurs Stand 2004;18:33-40.
6. Blencowe H, Cousens S, Modell B, Lawn J. Folic acid to
reduce neonatal mortality from neural tube disorders. Int J
Epidemiol 2010;39(Suppl 1):i110-21. Crossref
7. Wolff T, Witkop CT, Miller T, Syed SB; U.S. Preventive
Services Task Force. Folic acid supplementation for
the prevention of neural tube defects: an update of the
evidence for the U.S. Preventive Services Task Force. Ann
Intern Med 2009;150:632-9. Crossref
8. National Center for Immunization and Respiratory
Diseases. General recommendations on immunization—recommendations of the Advisory Committee on
Immunization Practices (ACIP). MMWR Recomm Rep
2011;60:26-7.
9. Wong VC, Ip HM, Reesink HW, et al. Prevention of the
HBsAg carrier state in newborn infants of mothers who are
chronic carriers of HBsAg and HBeAg by administration
of hepatitis-B vaccine and hepatitis-B immunoglobulin.
Double-blind randomised placebo-controlled study.
Lancet 1984;1:921-6. Crossref
10. Chou R, Smits AK, Huffman LH, Fu R, Korthuis PT; US
Preventive Services Task Force. Prenatal screening for HIV:
A review of the evidence for the U.S. Preventive Services
Task Force. Ann Intern Med 2005;143:38-54. Crossref
11. Wolff T, Shelton E, Sessions C, Miller T. Screening for
syphilis infection in pregnant women: evidence for
the U.S. Preventive Services Task Force reaffirmation
recommendation statement. Ann Intern Med
2009;150:710-6. Crossref
12. Lumley J, Chamberlain C, Dowswell T, Oliver S, Oakley
L, Watson L. Interventions for promoting smoking
cessation during pregnancy. Cochrane Database Syst Rev
2009;(3):CD001055. Crossref
13. Whitlock EP, Polen MR, Green CA, Orleans T, Klein J;
U.S. Preventive Services Task Force. Behavioral counseling
interventions in primary care to reduce risky/harmful
alcohol use by adults: a summary of the evidence for the
U.S. Preventive Services Task Force. Ann Intern Med
2004;140:557-68. Crossref
14. Britton C, McCormick FM, Renfrew MJ, Wade A, King SE.
Support for breastfeeding mothers. Cochrane Database
Syst Rev 2007;(1):CD001141. Crossref
15. Chung M, Raman G, Trikalinos T, Lau J, Ip S. Interventions
in primary care to promote breastfeeding: an evidence
review for the U.S. Preventive Services Task Force. Ann
Intern Med 2008;149:565-82. Crossref
16. Greenberg MT, Speltz ML, DeKlyen M. The role of
attachment in the early development of disruptive behavior
problems. Dev Psychopathol 1993;5:191-213. Crossref
17. Department of Health, HKSARG. The healthy eating food
pyramid—a guide to a balanced diet. Available from: http://www.cheu.gov.hk/eng/info/2plus3_12.htm. Accessed Mar
2015.
18. Thomas R, Zimmer-Gembeck MJ. Behavioral outcomes
of Parent-Child Interaction Therapy and Triple P-Positive
Parenting Program: a review and meta-analysis. J Abnorm
Child Psychol 2007;35:475-95. Crossref
19. Nowak C, Heinrichs N. A comprehensive meta-analysis
of Triple P-Positive Parenting Program using hierarchical
linear modeling: effectiveness and moderating variables.
Clin Child Fam Psychol Rev 2008;11:114-44. Crossref
20. de Graaf I, Speetjens P, Smit F, de Wolff M, Tavecchio L.
Effectiveness of the Triple P Positive Parenting Program
on behavioral problems in children: a meta-analysis. Behav
Modif 2008;32:714-35. Crossref
21. Effective strategies to support positive parenting in
community health centers: Report of the Working Group
on Child Maltreatment Prevention in Community Health
Centers. Washington, DC: American Psychological
Association; 2009.
22. Centre for Excellence and Outcomes in Children and
Young People’s Services. Improving children’s outcomes by
supporting parental physical and mental health. London:
Department for Education; 2011.
23. Clamp M, Kendrick D. A randomised controlled trial of
general practitioner safety advice for families with children
under 5 years. BMJ 1998;316:1576-9. Crossref
24. Physical Activity Guidelines Advisory Committee Report.
Washington, DC: US Department of Health and Human
Services; 2008.
25. Global Recommendations on Physical Activity for Health.
Geneva: World Health Organization; 2010.
26. Janssen I, Leblanc AG. Systematic review of the health
benefits of physical activity and fitness in school-aged
children and youth. Int J Behav Nutr Phys Act 2010;7:40. Crossref
27. Get up & grow: healthy eating and physical activity for
early childhood. Australia: Department of Health and
Aging; 2009. Available from: http://www.health.gov.au/internet/publications/publishing.nsf/Content/gug-carer-toc.
Accessed Mar 2015.
28. UK physical activity guideline. UK Department
of Health. Available from: http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_127931. Accessed
Mar 2015.
29. Guidelines for Preventive Activities in General Practice. 7th
ed. The Royal Australian College of General Practitioners;
2009.
30. US Preventive Services Task Force, Barton M. Screening
for obesity in children and adolescents: US Preventive
Services Task Force recommendation statement. Pediatrics
2010;125:361-7. Crossref
31. Williams SB, O’Connor EA, Eder M, Whitlock EP.
Screening for child and adolescent depression in primary
care settings: a systematic evidence review for the US
Preventive Services Task Force. Pediatrics 2009;123:e716-35. Crossref
32. Supporting smoking cessation: a guide for health
professionals. South Melbourne: The Royal Australian
College of General Practitioners; 2011.
33. American Academy of Pediatrics: Committee on Substance
Abuse. Alcohol use and abuse: a pediatric concern. Pediatrics 2001;108:185-9. Crossref
34. Preventive services for children and adolescents. 16th ed.
Institute for Clinical Systems Improvement; 2010.
35. Eisenberg ME, Olson RE, Neumark-Sztainer D, Story M, Bearinger LH. Correlations between family meals and psychosocial well-being among adolescents. Arch Pediatr
Adolesc Med 2004;158:792-6. Crossref