Hong Kong Med J 2015 Feb;21(1):84.e3–4
DOI: 10.12809/hkmj134189
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Inflammatory myoglandular polyps of the rectum
Akira Hokama, MD#; Chiharu Kobashigawa, MD#; Jiro Fujita, MD
Department of Infectious, Respiratory, and Digestive Medicine, University
of the Ryukyus, 207 Uehara, Nishihara, Okinawa 903-0215, Japan
# Currently at Department of Endoscopy, University of the Ryukyus, 207
Uehara, Nishihara, Okinawa 903-0215, Japan
Corresponding author: Dr Akira Hokama (hokama-a@med.u-ryukyu.ac.jp)
Case report
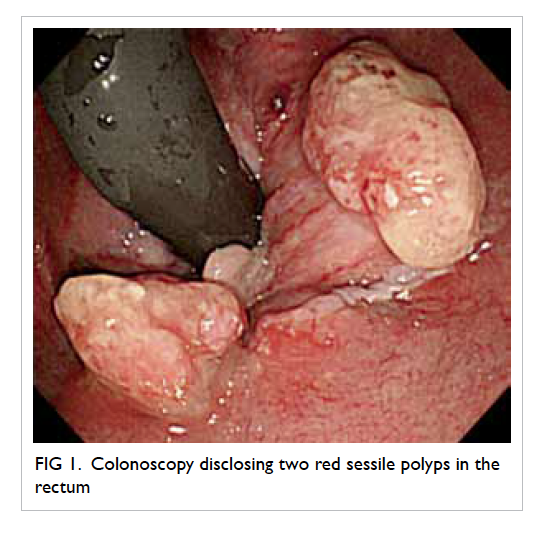
An 84-year-old woman with advanced pharyngeal
cancer underwent colonoscopy for intermittent
rectal bleeding in October 2012. Colonoscopy
disclosed two red sessile polyps in the rectum (Fig 1).
The larger one was spherical with a smooth surface,
measuring approximately 15 mm in diameter (Fig
2). Biopsy showed hyperplastic glands and marked
proliferation of smooth muscle cells in the lamina
propria, consistent with a diagnosis of inflammatory
myoglandular polyp (IMGP) [Fig 3]. The patient
denied colonoscopic treatment and stays in a hospice.
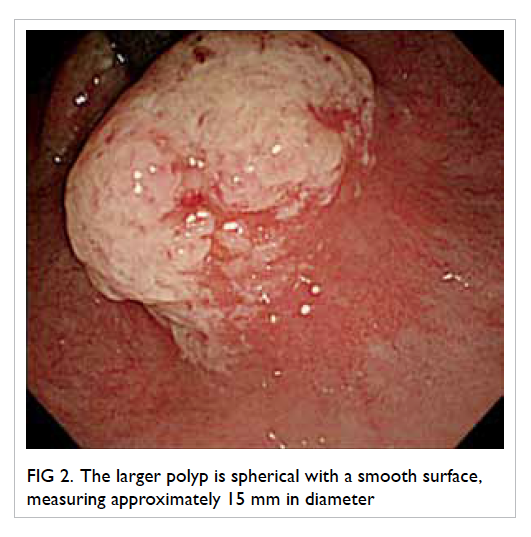
Figure 2. The larger polyp is spherical with a smooth surface, measuring approximately 15 mm in diameter
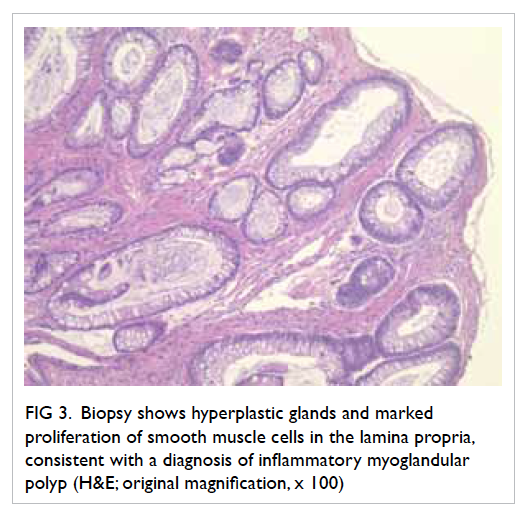
Figure 3. Biopsy shows hyperplastic glands and marked proliferation of smooth muscle cells in the lamina propria, consistent with a diagnosis of inflammatory myoglandular polyp (H&E; original magnification, x 100)
Inflammatory myoglandular polyp is a rare,
non-neoplastic polyp of the colorectum with
histological features of inflammatory granulation
tissue in the lamina propria, proliferation of
smooth muscle cells, and hyperplastic glands with
variable cystic changes.1 Since Nakamura et al1 first documented IMGP in 1992, only 60 cases of IMGPs
have been reported worldwide.2 As most IMGPs
are located in the rectum and the sigmoid colon, a
common symptom of the condition is haematochezia.
Although the causes of IMGP are obscure, chronic
trauma from the faecal stream and peristalsis may
contribute to its pathogenesis.1 With prolonged
irritation, small, sessile IMGPs can enlarge and
become pedunculated. Characteristic features include
hyperaemic surface with patchy mucous exudation
and erosion. Inflammatory myoglandular polyp
differs from other non-neoplastic polyps including
inflammatory cap polyps, inflammatory cloacogenic
polyps, juvenile polyps, inflammatory fibroid polyps,
polyps secondary to mucosal prolapse syndrome,
polypoid prolapsing mucosal folds of diverticular
disease in terms of its clinical and histopathological
features.2 Most IMGPs can be treated by endoscopic
resection. Because IMGP follows a benign course,
endoscopic resection might be unnecessary when
biopsy confirms the histopathological diagnosis.3
References
1. Nakamura S, Kino I, Akagi T. Inflammatory myoglandular
polyps of the colon and rectum. A clinicopathological
study of 32 pedunculated polyps, distinct from other types
of polyps. Am J Surg Pathol 1992;16:772-9. CrossRef
2. Meniconi RL, Caronna R, Benedetti M, et al. Inflammatory
myoglandular polyp of the cecum: case report and review
of literature. BMC Gastroenterol 2010;10:10. CrossRef
3. Hirasaki S, Okuda M, Kudo K, Suzuki S, Shirakawa A.
Inflammatory myoglandular polyp causing hematochezia.
World J Gastroenterol 2008;14:5353-5. CrossRef
Find HKMJ in MEDLINE: