Hong Kong Med J 2015 Feb;21(1):84.e1–2
DOI: 10.12809/hkmj134187
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Double-chambered right ventricle: a commonly overlooked diagnosis
Joe KT Lee, MRCP (UK), FHKAM (Medicine);
KL Tsui, FRCP (Edin, Glasg), FHKAM (Medicine)
Department of Medicine, Pamela Youde Nethersole Eastern Hospital, Chai
Wan, Hong Kong
Corresponding author: Dr Joe KT Lee (jktlee@gmail.com)
A 72-year-old woman presented with decreased
exercise tolerance since 2007. Based on a transthoracic
echocardiogram (TTE) in another hospital, the patient
was diagnosed to have perimembranous ventricular
septal defect (VSD) with pulmonary hypertension.
Upon referral to our unit in 2013, a more meticulous
TTE examination revealed a mid-cavitary stenosis in
the right ventricle (RV) which was best appreciated
in the parasternal short axis and the subcostal short
axis view (Figs 1 and 2). The systolic pressure gradient
measured by continuous-wave Doppler between the
two RV chambers was markedly elevated to 80 mm
Hg. There was also severe tricuspid regurgitation
with a dilated RV. The findings were confirmed on
a transoesophageal echocardiogram (TEE) and the
diagnosis was revised as double-chambered right
ventricle (DCRV) with perimembranous VSD (Fig
3). A right heart catheterization study showed a
stenotic band over the right ventricular outflow tract
(RVOT) [Fig 4]. The systolic pressure at the proximal
RV chamber was markedly elevated to 75 mm Hg.
However, we failed to manipulate the catheter
across the stenotic band to measure the pressure
gradient across the two chambers. The coronary
angiographic results were normal. The patient was
referred to cardiothoracic surgeons and open heart
surgery was undertaken. After right ventriculotomy,
the anomalous infundibular muscle bundle and a
small perimembranous VSD were identified. The
obstructive muscle bundle was resected and VSD
was repaired. The tricuspid valve was repaired by
means of annuloplasty. In postoperative TTE, the
previously noted high pressure gradient across the
RVOT was no longer present. The right ventricular
systolic pressure normalised to 15 mm Hg.
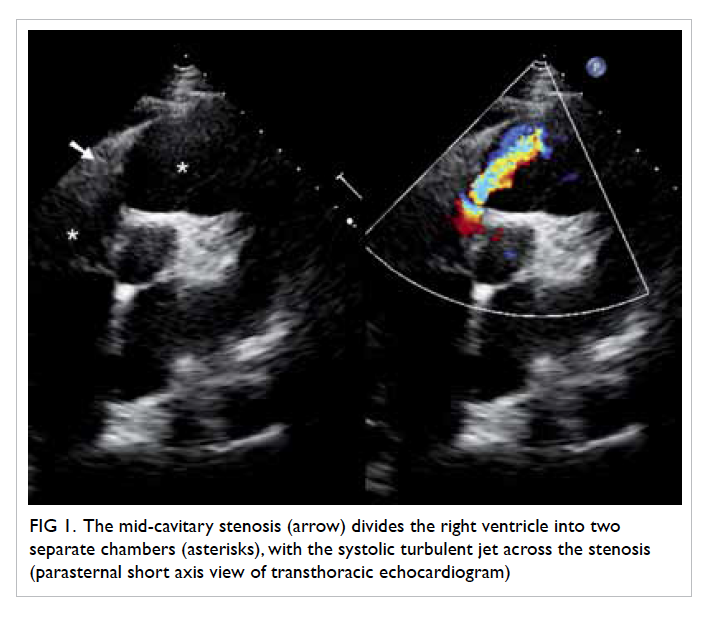
Figure 1. The mid-cavitary stenosis (arrow) divides the right ventricle into two separate chambers (asterisks), with the systolic turbulent jet across the stenosis (parasternal short axis view of transthoracic echocardiogram)
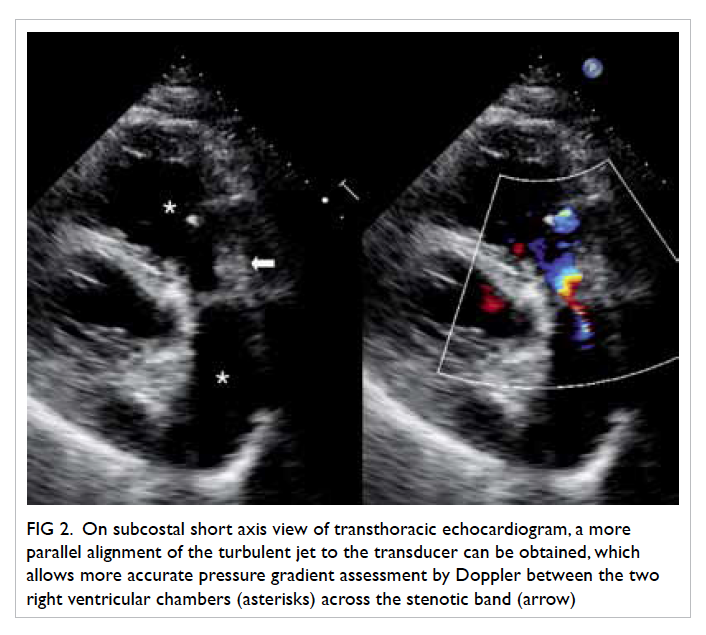
Figure 2. On subcostal short axis view of transthoracic echocardiogram, a more parallel alignment of the turbulent jet to the transducer can be obtained, which allows more accurate pressure gradient assessment by Doppler between the two right ventricular chambers (asterisks) across the stenotic band (arrow)
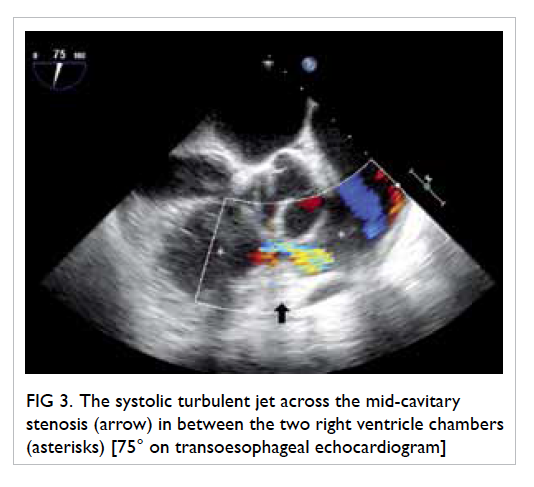
Figure 3. The systolic turbulent jet across the mid-cavitary stenosis (arrow) in between the two right ventricle chambers (asterisks) [75° on transoesophageal echocardiogram]
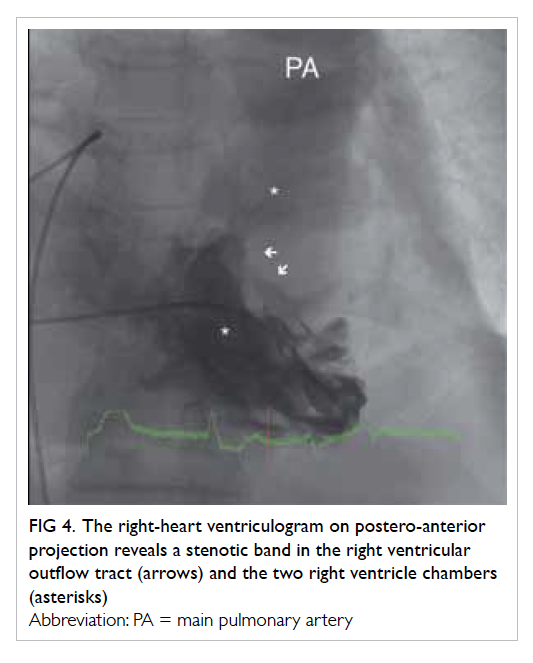
Figure 4. The right-heart ventriculogram on postero-anterior projection reveals a stenotic band in the right ventricular outflow tract (arrows) and the two right ventricle chambers (asterisks)
Discussion
Double-chambered RV is characterised by the
presence of an anomalous muscle bundle (AMB),
which divides the RV into two separate chambers,
namely, the proximal high-pressure and the distal
low-pressure chambers. The AMB is considered a
hypertrophied moderator band or the accentuated
septoparietal trabeculation.1 2 These congenital anatomical substrates and other acquired
haemodynamic factors lead to the development of
DCRV.
Double-chambered RV is an uncommon
condition and it is only seen in 0.5% to 2% of all cases
of congenital heart disease.3 Most cases are diagnosed
in childhood or adolescence before the age of 20
years. The occurrence in adults is rare and has only
been described in case reports and small case series.
About 80% to 90% of DCRV cases are associated with
VSD, or sometimes with other congenital cardiac
anomalies. Patients with DCRV usually present with
shortness of breath and decreased exercise tolerance,
but they may also have atypical symptoms such as
chest pain, dizziness, and syncope.
The irregular shape and retrosternal position
of RV, and its close proximity to the precordium
impose diagnostic difficulty by TTE, especially in
adults. Quite often, the mid-cavitary turbulent jet on
TTE is mistaken as an intracardiac shunt, and the
high RV systolic pressure is falsely interpreted as
pulmonary hypertension. In a case series, only 15.6%
of patients with DCRV could be correctly diagnosed
by TTE.3 A high clinical suspicion and awareness of
this clinical entity are required for precise diagnosis.
The subcostal view of TTE may sometimes provide
better visualisation of the RV and RVOT. It also
allows better alignment of the turbulent jet for
pressure gradient measurement. When TTE is not
confirmative, TEE and cardiac catheterization serve
as complementary tools. The use of cardiac magnetic
resonance imaging as non-invasive assessment is
now emerging as an alternative diagnostic modality
for DCRV.
Surgical repair of RV by resection of the AMB
is indicated in symptomatic patients, and it yields
excellent long-term haemodynamic and functional
results.4 Surgical treatment is also suggested in
asymptomatic patients who have significantly
elevated midventricular pressure gradient, that is,
>40 mm Hg as the obstruction can progress rapidly
over just a few years.5
References
1. Wong PC, Sanders SP, Jonas RA, et al. Pulmonary
valve-moderator band distance and association with
development of double-chambered right ventricle. Am J
Cardiol 1991;68:1681-6. CrossRef
2. Alva C, Ho SY, Lincoln CR, et al. The nature of the
obstructive muscular bundles in double-chambered right
ventricle. J Thorac Cardiovasc Surg 1999;117:1180-9. CrossRef
3. Hoffman P, Wojcik AW, Rozanski J, et al. The role of
echocardiography in diagnosing double chambered right
ventricle in adults. Heart 2004;90:789-93. CrossRef
4. Telagh R, Alexi-Meskishvili V, Hetzer R, et al. Initial
clinical manifestations and mid- and long-term results
after surgical repair of double-chambered right ventricle
in children and adults. Cardiol Young 2008;18:268-74. CrossRef
5. Oliver JM, Garrido A, Gonzalez A, et al. Rapid progression
of midventricular obstruction in adults with double-chambered
right ventricle. J Thorac Cardiovasc Surg
2003;126:711-7. CrossRef
Find HKMJ in MEDLINE:

