Hong Kong Med J 2015 Feb;21(1):52–60 | Epub 2 Jan 2015
DOI: 10.12809/hkmj144410
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
REVIEW ARTICLE
Allergy in Hong Kong: an unmet need in service provision and training
YT Chan, MB, BS, FHKAM (Pathology)1;
HK Ho, MB, BS, FHKAM (Paediatrics)2;
Christopher KW Lai, DM, FRCP3;
CS Lau, FRCP, FHKAM (Medicine)4;
YL Lau, MD, FHKAM (Paediatrics)2;
TH Lee, ScD, FRCP5;
TF Leung, MD, FRCPCH6;
Gary WK Wong, MD, FRCPC6;
YY Wu, MB, ChB, DABA&I3; The Hong Kong Allergy Alliance
1Division of Clinical Immunology, Department of Pathology and Clinical
Biochemistry, Queen Mary Hospital, Pokfulam, Hong Kong
2Department of Paediatrics and Adolescent Medicine, Queen Mary
Hospital, The University of Hong Kong, Pokfulam, Hong Kong
3Private practice, Hong Kong
4Division of Rheumatology and Clinical Immunology, Department of
Medicine, The University of Hong Kong, Pokfulam, Hong Kong
5Allergy Centre, Hong Kong Sanatorium & Hospital, Hong Kong
6Department of Paediatrics, The Chinese University of Hong Kong, Prince
of Wales Hospital, Shatin, Hong Kong
Corresponding author: Dr TH Lee (thlee@hksh.com)
Abstract
Many children in Hong Kong have allergic diseases
and epidemiological data support a rising trend.
Only a minority of children will grow out of their
allergic diseases, so the heavy clinical burden will
persist into adulthood. In an otherwise high-quality
health care landscape in Hong Kong, allergy services
and training are a seriously unmet need. There is one
allergy specialist for 1.5 million people, which is low
not only compared with international figures, but also
compared with most other specialties in Hong Kong.
The ratio of paediatric and adult allergists per person
is around 1:460 000 and 1:2.8 million, respectively,
so there is a severe lack of adult allergists, while the
paediatric allergists only spend a fraction of their
time working with allergy. There are no allergists
and no dedicated allergy services in adult medicine
in public hospitals. Laboratory support for allergy
and immunology is not comprehensive and there is
only one laboratory in the public sector supervised
by accredited immunologists. These findings clearly
have profound implications for the profession
and the community of Hong Kong and should be
remedied without delay. Key recommendations are
proposed that could help bridge the gaps, including
the creation of two new pilot allergy centres in a hub-and-spoke model in the public sector. This could
require recruitment of specialists from overseas to
develop the process if there are no accredited allergy
specialists in Hong Kong who could fulfil this role.
Introduction
There is a global epidemic of allergic diseases in
the developed world and Hong Kong has not been
spared. This review provides an overview of the
epidemiology of allergic diseases in Hong Kong
and matches it to the provision of local health care
services as well as training in allergy.
How common are allergic diseases in Hong Kong?
The International Study of Asthma and Allergies
in Childhood (ISAAC)1 2 3 4 5 6 and other local studies7 8 9 10 11
provide data on the prevalence and changing trends
for some allergic diseases in Hong Kong. The ISAAC
was a multi-country cross-sectional survey that
provided a global epidemiological map of eczema,
asthma, and rhinoconjunctivitis in 1995, 2000,
and 2003. Children aged 6 to 7 years and 13 to 14
years were studied. The ISAAC Phase Three was a
repetition of the ISAAC Phase One that aimed to
evaluate the possible trend of disease prevalence
after a period of 5 to 10 years.
In 2001, the prevalence of those who had ever
been diagnosed with asthma in 6- to 7-year-olds
was 7.9%. This reflected an increase of about 0.04%
compared with 1995. In 2002 the prevalence of
having asthma ever in 13- to 14-year-olds was 10.1%,
representing a decrease in prevalence of 0.15% per
year since 1995.
In 2001, the prevalence of lifetime eczema in
6- to 7-year-olds was 30.7% and current eczema was
4.6%. This reflected an increase in the current eczema
prevalence of 0.12% per year since 1995. In 13- to
14-year-olds, the prevalence of lifetime eczema was
13.4% and that of current eczema was 3.3%. This reflected
an increase of 0.08% per year since 1995.
In 2002, the rhinoconjunctivitis prevalence in
13- to 14-year-olds was 22.6% and showed a decrease
of 0.2% per year since 1995. Similar figure for 6- to
7-year-olds was 17.7% in 2001 and this represented
an increase of 0.7% per year since 1995.
The Asthma Insights and Reality in Asia-Pacific
Study was conducted twice in Asian countries,
including mainland China, Hong Kong, Korea,
Malaysia, The Philippines, Taiwan, and Vietnam,
to gain insight into asthma management.12 In the
first survey of more than 3000 adults and children,
more than 40% of asthmatic patients had at least one
hospitalisation or visit to the emergency department
for acute exacerbation. Inhaled corticosteroid use
was reported by only 13.6% of the respondents.
Another study performed 10 years after the first
survey showed that less than 5% of patients achieved
a level of complete asthma control, while more than
one third were in the uncontrolled asthma category.
Patients tended to overestimate their level of control
and tolerated a high degree of impairment of their
daily activities.12 13 14 Most participants younger than
16 years had inadequately controlled asthma (53.4%
‘uncontrolled’ and 44.0% ‘partly controlled’). The
demands for urgent health care services (51.7%) and
use of short-acting β-agonists (55.2%) were high.15
There are little epidemiological data on
asthma and allergy in Hong Kong adults. In a
review of data from local public hospitals in 2005,
asthma ranked fourth and fifth highest as a cause of
respiratory hospitalisations (5.7%) and respiratory
inpatient bed-days (2.6%), respectively.16 The overall
crude hospitalisation rate for asthma in 2005 was
76/100 000, and was high at both extremes of age. The
age-standardised mortality rate of asthma increased
between 1997 (1.33/100 000) and 1998 (1.82/100 000),
but decreased thereafter to 1.4/100 000 in 2005. The
overall annual change in asthma mortality was not
significantly different between 1997 and 2005. The
prevalence of current wheeze increased from 7.5%
in 1991/1992 to 12.1% in 2003/2004 among people
older than 70 years; the corresponding figures for
asthma were 5.1% and 5.8%.17
A number of studies have examined the
prevalence of food allergies and adverse food
reactions in a wide age range of Hong Kong
children.9 10 11 18 In 2009, parent-reported adverse
reactions in 2- to 7-year-olds was 8.1%. A study
involving children aged 7 to 10 years reported in
2010 that ‘probable’ food allergy in Hong Kong
was 2.8%.10 In 2012, the prevalence of food allergy in
children from birth to 14 years was 4.8%, of which
shellfish was by far the commonest food causing
allergic symptoms, alongside egg, milk, peanuts, and
fruits.10
Children with food allergies have 2 to 4 times
higher rates of co-morbid conditions, including
asthma, rhinoconjunctivitis, and eczema. Strikingly
700/100 000 of the population (15.6% of children
with food allergies) aged 14 years or younger are
estimated to be at risk for anaphylaxis, which is high
relative to other countries. Almost 50% of cases are
estimated to be caused by foods, with drug allergy
also being a cause.11
Regarding other allergic diseases, Leung et
al19 reported glove-related symptoms in nearly
one third of 1472 employees in a teaching hospital
in Hong Kong. Most of these allergies could be
classified as glove dermatitis, whereas only 3.3% had
symptoms suggestive of latex allergy. About 7% of
133 participants had positive skin prick testing to
one or more of the five latex extracts.
How does Hong Kong compare
with the rest of the world in the
number of allergy specialists?
There are only four immunology and allergy
specialists (Medical Council Specialist Registration
S34) in Hong Kong. Two of these clinicians, both of
whom were trained abroad, are in private practice
and the other two are not involved in allergy practice.
There are no registered allergy specialists in adult
medicine in public hospitals.
There are six specialists in Paediatric
Immunology and Infectious Diseases (PIID; Medical
Council Specialist Registration S56) of whom two
work full time and four work part time, mainly in an
allergy/immunology practice in the Hospital Authority
(HA) hospitals/university sector. There is another
PIID specialist working in private practice. Most of
these clinicians only work part time on allergy.
Many patients with allergic diseases in Hong
Kong are treated by non-allergy specialists, such as
general practitioners, or specialists in dermatology,
respiratory medicine, ear nose and throat medicine,
and paediatrics. While these excellent clinicians
undoubtedly have experience in looking after
patients with allergies, it is unclear how many have
received formal training in managing complex
multi-system allergies or whether their continuous
professional development (CPD) activities include
allergy.
If one assumes that PIID specialists spend on
average 40% of their working week (5.5 days) on
allergy, irrespective of whether they are full or part
time (a generous estimate), then Hong Kong has 2
full-time equivalent (FTE) adult allergists and 2.8
FTE PIID specialists consulting for allergy. The
overall ratio is therefore estimated to be around one
allergist to 1.46 million population in Hong Kong,
which is near the bottom of the world league table
published by the World Allergy Organization
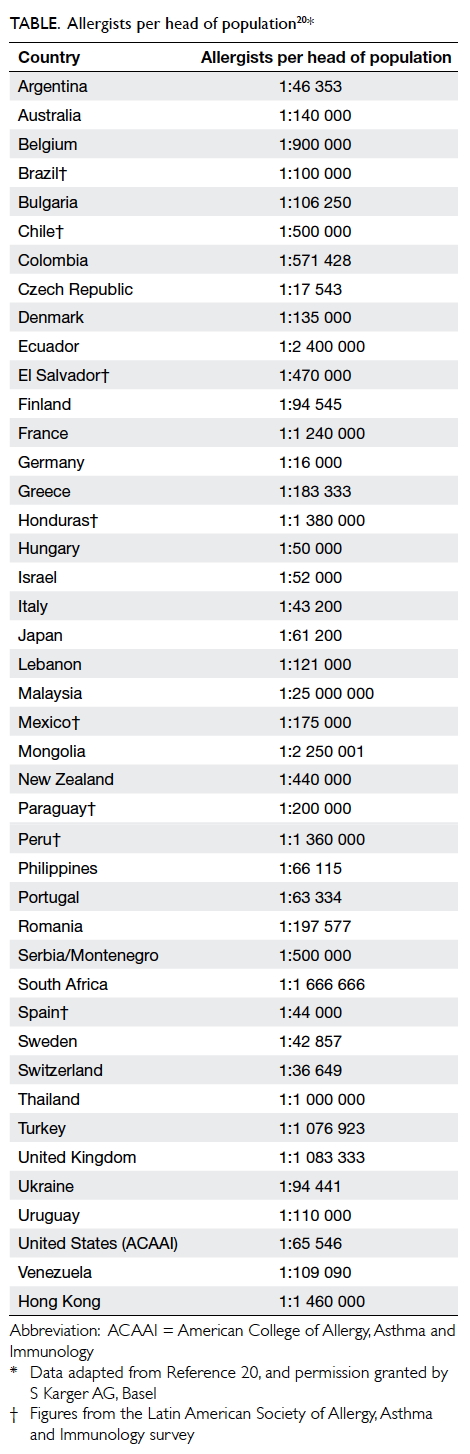
(Table20).
There is a stark contrast in Hong Kong
between the level of service provision for children
and that for adults. The ratio of paediatric and adult
allergists per head of population is around 1:460 000
(assuming there are about 1.3 million children in
Hong Kong who are younger than 18 years) and
1:2.8 million (assuming there are about 5.7 million
adults), respectively. There are no allergists for adult
patients in public hospitals. The very low numbers
of allergists (4.8 FTE) compares unfavourably with
other specialties in Hong Kong, for example, there
are 226 cardiologists, 164 gastroenterologists, 162
respiratory physicians, 190 otorhinolaryngologists,
and 92 dermatologists. These data, combined with
the average waiting times at public hospitals of 6
to 9 months for a new allergy appointment, clearly
indicate that the demands for allergy services are
unmet. The disease burden cannot be absorbed by
the private sector as there are also very few private
allergists.
Laboratory support is essential for the
good practice of allergy and immunology. There
are two Hong Kong Medical Council–registered
immunologists (S44) who have also received some
allergy training. One of them directs a public
laboratory service in immunology and allergy as well
as providing a limited service for drug allergy, while
the other is not involved with allergy. Their budget
does not allow a comprehensive menu of relevant
tests to support the specialty.
In countries where there are more allergists
per head of population than in Hong Kong, patients
still consult non-allergy specialists instead of an
allergist, even for a condition that often has an
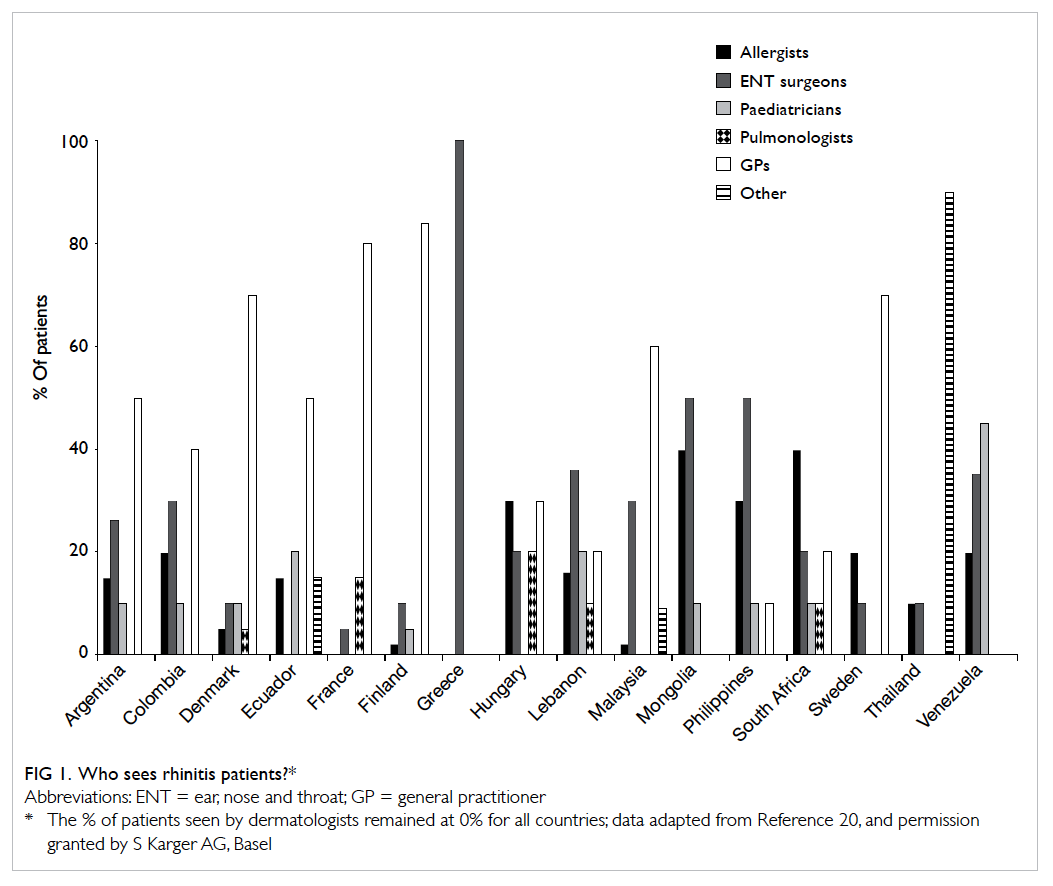
allergic cause such as rhinitis (Fig 120).This suggests
that there is a relative global lack of understanding
of what allergists can offer in health care. Clearly
much needs to be done in public and professional
education.
In the absence of allergists, patients may
suffer because they may find it hard to get state-of-the-art medicine and diagnostics. Pharmaceutical
companies are less likely to register their products
in a country where the drugs will be prescribed only
rarely. Furthermore, there is a high probability that
unproven diagnostic procedures and therapies could
be introduced if mainstream medicine is unavailable,
or conventional tests are used inappropriately.21
Finally, with a lack of allergy specialists, it becomes
difficult to train future generation of clinicians,
researchers, and teachers in allergy.
What is the provision of allergy services in public hospitals in Hong Kong?
Current situation for children
There are 12 acute paediatric units admitting children
and adolescents for various acute exacerbations of
diseases, including systemic allergic reactions and
acute asthmatic attacks. The level of acute care is
comprehensive and includes intensive care unit
support when indicated. Data from the HA suggest
that one in 10 patients with anaphylaxis attending
acute emergency departments has been admitted to
a paediatric intensive care unit.22
Ambulatory and out-patient follow-ups,
however, are sometimes fragmented, especially for
the prevention of anaphylaxis and investigation
to identify allergens. Adrenaline auto-injector (eg
EpiPen [Dey LP, Napa, California, US]) availability
is very limited, although much improved recently,
probably as the result of an audit report identifying
the unmet need.22
Only four hospitals have designated allergy
clinics to investigate food and drug allergy (Queen
Mary Hospital [QMH], Prince of Wales Hospital
[PWH], Princess Margaret Hospital [PMH],
and Queen Elizabeth Hospital [QEH]). Some
paediatricians with gastro-intestinal training look
after patients with non-immunoglobulin E (IgE)–mediated food allergy with predominant gastro-intestinal symptoms.
Most of the paediatric units in Hong Kong have
asthma clinics that are run by paediatricians with
respiratory training. Care of patients with allergic
rhinoconjunctivitis is largely provided by general
paediatricians in conjunction with other organ
specialists such as ear, nose and throat surgeons
and ophthalmologists; there are long waiting times,
ranging from 6 to 12 months.
Five hospitals have dermatology clinics (QMH,
PWH, United Christian Hospital, Caritas Medical
Centre, and Pamela Youde Nethersole Eastern
Hospital) run by paediatricians with dermatology
training, but also treating some patients with
allergies.
Currently, there is one single immunology/allergy public laboratory service in QMH that
provides limited numbers of specific IgE, human
leukocyte antigen, and tryptase tests. Clinical
investigational laboratories for in-vivo allergen skin
tests and challenge protocols are run by specialists
in PIID or paediatrics. Food and drug challenges
are provided at QMH and PWH on a regular basis,
but may be occasionally provided by other hospitals
such as QEH, PMH, and Kwong Wah Hospital. The
waiting time is generally about 6 months. There are
no commonly accepted local challenge protocols, so
those used by internationally recognised paediatric
allergy centres are followed.
Currently, the four PIID centres have two FTE
staff plus four part-time staff who work mainly on
food and drug allergies. The trained dietician and
nurses work only on a part-time basis. There is also
one private PIID specialist.
Clinical guidelines
Local anaphylaxis guidelines have been drafted and
are pending approval and implementation. The Hong
Kong College of Paediatricians has issued guidelines
to improve care for atopic dermatitis. Different
hospitals may have different in-house guidelines for
asthma or they may be adopted from international
guidelines.
Allergen immunotherapy
Allergen immunotherapy is very limited in public
service. The reasons are multifactorial and include
affordability, availability, and accessibility.
Resources
Lack of central funding may seem to be a hindrance
to provision of allergy services, but the real problem
is the shortage of skilled staff. Many trained nurses
experienced in skin testing and allergy education
have left their jobs or have been redeployed to other
areas. To cater for the current service demands and
to achieve reasonable waiting times, more staff need
to be trained urgently, for instance, a resident trainee,
advanced practice nurses, and even clerical support.
Current situation for adults
There is currently no formal allergy clinical service
provided in the public sector for adults. Clinicians,
including a few dermatologists, respiratory
physicians and otolaryngologists, who have an
interest in allergy provide an ad-hoc service to
patients with various allergic disorders. Limited
skin prick tests are provided. There are, however, no
specialty nurses or technicians specially trained in
this area.
In 2013, the Division of Rheumatology and
Clinical Immunology, together with the Division
of Clinical Immunology (Pathology) set up a Drug
Allergy Clinic at QMH to provide consultations
for Hong Kong West Cluster patients. Because
of resource restrictions, these consultations are
limited to the diagnosis and confirmation of general
anaesthetic and antibiotic allergies.
Hong Kong has produced only one locally
trained immunologist who is an HIV (human
immunodeficiency virus) specialist currently
working in the Department of Health. There have
been no trainees in allergy and immunology since
1998.
Drug allergies
Data retrieved on 30 June 2013 from an analysis of HA data (personal communication) indicate that almost 400 000 patients have drug allergy, with
44 018 having three or more drug allergies. Almost
5000 patients (mainly adults) have three or more
antibiotic allergies. This is a huge potential clinical
workload that impacts on many other specialties,
and is a growing area of allergic disease that needs to
be addressed urgently.
Laboratory support services for allergy/immunology
Only one laboratory service for allergy/immunology in Hong Kong is directed by accredited
immunologists in the public sector (at QMH). The
service cannot offer a complete portfolio of tests
because of budgetary constraints.
Training
Paediatric Immunology and Infectious Diseases
The first Fellowships of the subspecialty of PIID were
conferred in 2012 (Medical Council Registration
S56). Among the first 12 Fellows, five work
principally in the field of immunology and allergy.
Paediatric units of four regional hospitals (QMH/The University of Hong Kong [HKU], PWH/The
Chinese University of Hong Kong [CUHK], PMH,
and QEH) are accredited to be the training centres
and they have formed a training network. Allergy is
an integral part of the PIID programme.
Higher training in allergy in adult medicine
Allergy and hypersensitivity is one of the five areas
of knowledge requirement for the training in allergy
and immunology under the Hong Kong College of
Physicians (HKCP). The other four areas include
autoimmune and immune complex diseases, primary
and secondary immunodeficiency, transplantation,
and lymphoproliferative diseases. Training in adult
allergy is hampered by the lack of trainers and the
lack of an allergy clinical service in the public sector.
Immunology
Training of immunology is under the Hong Kong
College of Pathologists (HKCPath). The goal of
training is to produce specialist immunologists who
are able to direct a laboratory service in clinical
immunology and tissue typing, to advise clinicians
on the management of immunological disorders,
including allergy, autoimmunity, immunodeficiency,
and malignancy of the immune system. At present
such training is only available at QMH where there
are two immunologists.
Recommendations
With the introduction of potent targeted biologics,
greater understanding of the genetics and
epigenetics determining allergic disease expression,
improved strategies and vaccines for allergen-specific
desensitisation, novel approaches to allergy
prevention, and the advent of an era of stratified
medicine, the need for more allergists, allergy
services, research, and trainees in the specialty have
never been more urgently required. In an otherwise
high-quality health care landscape in Hong Kong,
allergy services and training are a seriously unmet
need. The deficiencies should be remedied without
delay for the benefit of the patient community.
The recommendations described below are
adapted from a recent authoritative report about
allergy23 and should also be seen in the context of
the declaration of the World Allergy Organization in
2013.24
Model and location
(1) We recommend that urgent advice is sought
from the major stakeholders on how one might
remedy the unmet need for allergy services
and training in Hong Kong.
(2) We recommend that the best model for allergy
service delivery is a ‘hub-and-spoke’ model
(Fig 223). The ‘hub’ would act as a central point
of expertise with outreach clinical services,
education, and training provided to doctors,
nurses, and allied health care professionals in
primary and secondary care (the ‘spokes’). In
this way, knowledge regarding the diagnosis
and management of allergic conditions could
be disseminated throughout the region. The
hub and spokes in its entirety forms the ‘allergy
centre’. The hub should lead and coordinate the
activities of the entire centre.
(3) Each hub should have an allergy service
both for adults and for children to share in
knowledge transfer and resources. In addition
to hubs, a network of satellite allergy services
could be established at different hospitals (for
instance by changing the emphasis of one or
two existing clinics a week designated for
respiratory medicine, otorhinolaryngology,
and/or dermatology to become allergy clinics),
which can then link to one of the allergy hubs
for academic, clinical, and educational support.
This solution might not incur substantially
more resources, as the complex multi-system
allergy cases could be transferred from the
other clinics and managed in a new dedicated
allergy service.
(4) We recommend that paediatric and adult
services in an allergy centre should each be
led by an allergy specialist and each should
be supported by at least one other clinical
colleague (another allergy specialist or an organ
specialist with a special interest in allergy),
at least one trainee, specialist dietician and
nursing support, and a technician for routine
allergy testing, counselling, and education.
(5) The hub forming the allergy centre will be
collaborating, not competing, with single organ
specialists or with general paediatricians,
internists, and general practitioners. It is
envisaged that the tertiary allergy centres
would work together with other colleagues to
provide joint, integrated, and holistic care for
the most complex allergy cases, which are often
characterised by multi-system involvement. To
facilitate this interaction, it is recommended
that clear criteria are defined for the types
of patients that could be referred to tertiary
specialist allergy centres.
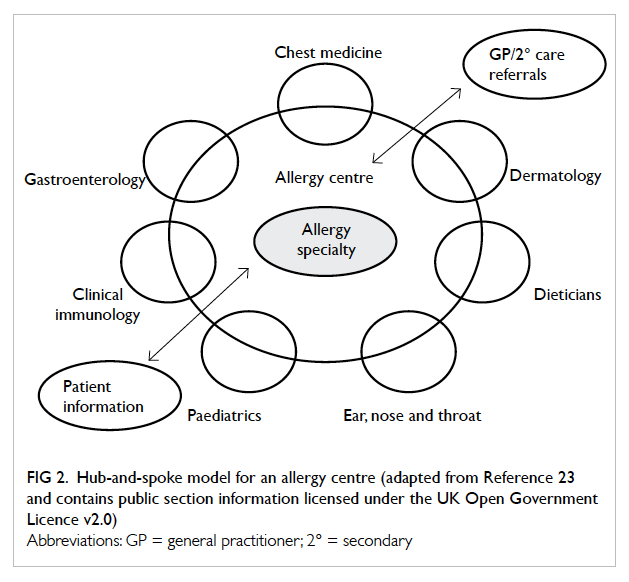
Figure 2. Hub-and-spoke model for an allergy centre (adapted from Reference 23 and contains public section information licensed under the UK Open Government Licence v2.0)
Adult allergy
(1) We recommend that two pilot allergy centres
are created by recruiting allergy specialists
(from overseas if necessary) to start the
services and to oversee a training programme.
(2) We recommend that each of the new
appointees is a joint appointment between the
HA and a university. Each appointee should be
supported by three trainees, a specialist nurse,
and a dietician.
(3) We recommend that the two pilot allergy
centres should be located at QMH/HKU and
PWH/CUHK (hubs), so that Hong Kong, Kowloon,
and the New Territories are covered. Two
pilot centres are required because of the heavy
burden of allergic disease and the capacity of a
solitary centre in Hong Kong would very soon
become overextended. Both QMH and PWH
have a long distinguished history of looking
after children with allergic and immunological
diseases, but both lack a dedicated allergist
in adult medicine. Creation of an allergy
centre that integrates existing strengths in
paediatric clinical/academic/education in
allergy with a new adult clinical/academic/education allergy service would be a major
catalyst to bridging the obvious gaps in service
and academic provision. Formal designation
of both hospitals as pilot allergy centres
could also provide formal encouragement to
hospital and university management for some
internal realignment of resources. Finally
creating these innovative allergy centres could
provide significant opportunities to attract
private funding from benefactors to grow the
discipline subsequently.
(4) We recommend that metrics for success of
each pilot centre be predefined and progress in
the first 5 years be assessed against those goals.
If the pilot is successful, then the model should
be continued and could even be extended to
other suitable clinical/academic centres.
(5) We recommend that the HKCP training
curriculum for immunology and allergy is
updated as soon as possible. In addition, we
suggest that the HKCP and HKCPath consider
creating an intercollegiate training programme
in immunology and allergy to produce clinical
immunologists who will direct allergy/immunology laboratories and consult for
allergic patients. This can be extended to
other colleges and cross-college training is
encouraged by the Hong Kong Academy of
Medicine. In due course, a core curriculum in
allergy could be shared by all interested colleges
in addition to a college-specific curriculum.
This model is already being explored for subspecialty
training in genetics and genomics
among some academy colleges.
(6) We recommend the training of allergy as a main
subject to be included in the college training
guidelines in allergy and immunology and four
allergy and immunology trainees majoring in
allergy are recruited every 4 years.
Paediatric allergy
(1) It is envisaged to develop an immunology and
allergy centre at the Hong Kong Children’s
Hospital (HKCH) for management of complex
allergy cases from 2018 onwards (a hub). A
team of core medical and nursing staff will be
based at HKCH, but will also run an outreach
programme by linking up with other network
hospitals.
(2) When the immunology and allergy centre at
the HKCH is operational, there will need to be
some reorganisation with parts of the top-tier
paediatric allergy services in the ‘hub’ hospitals
being moved to the HKCH (which will then
become the new hub), leaving satellite services
in the previous ‘hub’ hospitals (the spokes) in
situ.
(3) To facilitate a smooth transition to the HKCH,
we recommend at least four to five FTE PIID
specialists majoring in allergy/immunology
to be appointed to run the top-tier service at
the HKCH, to provide training and conduct
local relevant audit/research (hub). A further
12 PIID specialists will be required to provide
step-down and secondary services in both the
training (PMH, PWH, QEH, QMH) and non-training
(other HA paediatric units) posts for
the specialty and general paediatrics (spokes).
(4) We recommend that common protocols,
guidelines, care pathway, and a referral
network, especially for complex cases, should
be agreed and formally created.
(5) We recommend that four PIID trainees are
recruited every 3 years, of which at least
two resident specialists majoring in allergy/immunology should be trained. This will
maintain a sustainable public workforce for
specialty development and cover for normal
turnover. It should then be possible to produce
12 PIID specialists in three cycles (around
9 years), of whom 50% will have majored in
allergy/immunology with the rest majoring in
infectious diseases. Therefore, the estimated
total required workforce for PIID in the public
sector for the hub-and-spoke model could be
18 to 20 with eight in the hub (four to five in
allergy and immunology and two to three in
infectious diseases) and about 12 in the spokes
working in both the specialty and general
paediatrics.
(6) We recommend that allergy is added to the
title of the PIID training programme so it will
become a PIAID (paediatric immunology allergy and
infectious diseases) programme and
the paediatric discipline should also be so
named.
Drug allergy
Drug allergy is common and constitutes a major
clinical problem, which needs to be managed by
allergy specialists. We recommend resources to
be made available to establish two separate supraregional
drug allergy services at QMH and PWH (as
they already have a limited service) to cover Hong
Kong Island and Kowloon/New Territories. This
could be part of the new pilot centres.
Laboratory support
We recommend that two supraregional
laboratories for Hong Kong should be created with
a focus on drug and food allergy that are directed by
accredited immunologists. The laboratories should be
adequately funded so that they have sufficient manpower,
equipment, and budget for reagents to widen
the scope of routine laboratory services to include
tests for specific IgE to a wide spectrum of whole allergen
extracts and to allergen components, basophil
activation tests, and lymphocyte function tests. This
can be incorporated into existing laboratory support
at QMH and PWH with only a relatively modest
increase in resources. These laboratories could then
support the new pilot centres.
Education
We recommend that collaboration is established
between the Hong Kong Institute of Allergy (as
the professional platform) and Hong Kong Allergy
Association (as the allergy charity) to create an agenda
for professional CPD (such as regular workshops)
as well as engaging and educating the public about
allergy. These organisations are strongly encouraged
to involve other professional societies and charities
as appropriate when designing their strategies.
Schools
(1) We recommend that the appropriate
Government department should audit the
level of allergy training staff in schools receive,
and consider taking urgent remedial action to
improve this training where required.
(2) We recommend that the Government should
review the desirability of schools holding one
or two generic auto-injectors.
Air quality
Solving the urban air pollution problem is a huge
challenge. Bold, realistic, and moral leadership by
national leaders is required to address this increasingly
important public health issue. We recommend
that it is essential to develop effective strategies
to reduce pollution, to engage the public, and to
monitor whether the strategies result in a significant
improvement in the prevalence of pollution-related
diseases in Hong Kong and mainland China.
Conclusions
Epidemiological data support a rising trend in
many allergic diseases. The provision of services
and training for specialists in allergy is mismatched
with disease burden and there is a large unmet
need that should be remedied without delay. Key
recommendations are proposed that could help
bridge the gaps, including the creation of two
pilot allergy centres in a hub-and-spoke model in
the public sector. This could require recruitment
of specialists from overseas to start the process in
the likely event that there are no accredited allergy
specialists in Hong Kong who could fulfil this role in
the short term.
Declarations of interest
Drs CKW Lai, CS Lau, YY Wu, and Prof TF Leung
are consultants or serve on advisory boards and/or
receive travel expenses and lecture fees to attend
international meetings from various pharmaceutical
companies including GlaxoSmithKline, AstraZeneca, Takeda, Mundipharma, Boehringer, ALK-Abello, AbbVie, Bristol-Myers Squibb, Celltrion, Janssen, Novartis, Pfizer, Roche, Sanofi, and Union Chimique Belge. Dr TH Lee is President of the Hong Kong Institute of Allergy and Honorary Clinical Professor,
The University of Hong Kong. Dr Marco Ho is
Chairman of the Hong Kong Allergy Association.
The Hong Kong Allergy Alliance is a group of individuals
with an interest in allergy drawn from academia, HA
hospitals, private practitioners, representatives from
the HA, Hong Kong Institute of Allergy, Hong Kong
Thoracic Society, Hong Kong Allergy Association,
patients, and drug company representatives from
ALK.
References
1. Worldwide variation in prevalence of symptoms of asthma,
allergic rhinoconjunctivitis, and atopic eczema: ISAAC. The
International Study of Asthma and Allergies in Childhood
(ISAAC) Steering Committee. Lancet 1998;351:1225-32. CrossRef
2. Worldwide variations in the prevalence of asthma
symptoms: the International Study of Asthma and Allergies
in Childhood (ISAAC). Eur Respir J 1998;12:315-35. CrossRef
3. Asher MI, Montefort S, Björkstén B, et al. Worldwide time trends in the prevalence of symptoms of asthma, allergic
rhinoconjunctivitis and eczema in childhood: ISAAC
Phases One and Three repeat multicountry cross-sectional
surveys. Lancet 2006;368:733-43. CrossRef
4. Pearce N, Aït-Khaled N, Beasley R, et al. Worldwide trends
in the prevalence of asthma symptoms: phase III of the
International Study of Asthma and Allergies in Childhood
(ISAAC). Thorax 2007;62:758-66. CrossRef
5. Williams H, Stewart A, von Mutius E, Cookson W,
Anderson HR; International Study of Asthma and Allergies
in Childhood (ISAAC) Phase One and Three Study Groups.
Is eczema really on the increase worldwide? J Allergy Clin
Immunol 2008;121:947-54.e15.
6. Lai CK, Beasley R, Crane J, Foliaki S, Shah J, Weiland S;
International Study of Asthma and Allergies in Childhood
Phase Three Study Group. Global variation in the
prevalence and severity of asthma symptoms: phase three
of the International Study of Asthma and Allergies in
Childhood (ISAAC). Thorax 2009;64:476-83. CrossRef
7. Wong GW, Leung TF, Ko FW. Changing prevalence of
allergic diseases in the Asia-pacific region. Allergy Asthma
Immunol Res 2013;5:251-7. CrossRef
8. Wong GW, Leung TF, Ma Y, Liu EK, Yung E, Lai CK.
Symptoms of asthma and atopic disorders in preschool
children: prevalence and risk factors. Clin Exp Allergy
2007;37:174-9. CrossRef
9. Smit DV, Cameron PA, Rainer TH. Anaphylaxis
presentations to an emergency department in Hong Kong:
incidence and predictors of biphasic reactions. J Emerg
Med 2005;28:381-8. CrossRef
10. Leung TF, Yung E, Wong YS, Lam CW, Wong GW. Parent-reported
adverse food reactions in Hong Kong Chinese
preschoolers: epidemiology, clinical spectrum and risk
factors. Pediatr Allergy Immunol 2009;20:339-46. CrossRef
11. Ho MH, Lee SL, Wong WH, Ip P, Lau YL. Prevalence of
self-reported food allergy in Hong Kong children and
teens—a population survey. Asian Pac J Allergy Immunol
2012;30:275-84.
12. Lai CK, De Guia TS, Kim YY, et al. Asthma control in the
Asia-Pacific region: the Asthma Insights and Reality in
Asia-Pacific Study. J Allergy Clin Immunol 2003;111:263-8. CrossRef
13. Rabe KF, Adachi M, Lai CK, et al. Worldwide severity and
control of asthma in children and adults: the global asthma
insights and reality surveys. J Allergy Clin Immunol
2004;114:40-7. CrossRef
14. Zainudin BM, Lai CK, Soriano JB, Jia-Horng W, De Guia
TS; Asthma Insights and Reality in Asia-Pacific (AIRIAP)
Steering Committee. Asthma control in adults in Asia-Pacific. Respirology 2005;10:579-86. CrossRef
15. Wong GW, Kwon N, Hong JG, Hsu JY, Gunasekera KD.
Pediatric asthma control in Asia: phase 2 of the Asthma
Insights and Reality in Asia-Pacific (AIRIAP 2) survey.
Allergy 2013;68:524-30. CrossRef
16. Chan-Yeung M, Lai CK, Chan KS, et al. The burden of
lung disease in Hong Kong: a report from the Hong Kong
Thoracic Society. Respirology 2008;13 Suppl 4:S133-65. CrossRef
17. Vital statistics on mortality. Department of Health website: http://www.healthyhk.gov.hk/phisweb/en/health_info/vit_stat/mortality/. Accessed Sep 2014.
18. Wong GW, Mahesh PA, Ogorodova L, et al. The
EuroPrevall-INCO surveys on the prevalence of food
allergies in children from China, India and Russia: the
study methodology. Allergy 2010;65:385-90. CrossRef
19. Leung R, Ho A, Chan J, Choy D, Lai CK. Prevalence of latex
allergy in hospital staff in Hong Kong. Clin Exp Allergy
1997;27:167-74. CrossRef
20. Warner JO, Kaliner MA, Crisci CD, et al. Allergy practice
worldwide: a report by the World Allergy Organization
Specialty and Training Council. Int Arch Allergy Immunol
2006;139:166-74. CrossRef
21. Wüthrich B. Unproven techniques in allergy diagnosis. J
Investig Allergol Clin Immunol 2005;15:86-90.
22. Ho MH, Wong LM, Ling SC, et al. Identifying the service gaps in the management of severe systemic allergic reaction/anaphylaxis by Paediatrics Departments of the Hospital Authority. HK J Paediatr (new series) 2010;15:186-97.
23. House of Lords Science and Technology Committee.
Allergy: HL 166-I, 6th Report of Session 2006-07—Volume
1. The Stationery Office Ltd; 2007.
24. Pawankar R, Canonica GW, Holgate ST, Lockey RF. WAO
White book on allergy 2011-2012: Executive summary.
WAO White book on allergy. Milwaukee, Wisconsin:
World Allergy Organization; 2011.
Find HKMJ in MEDLINE: