DOI: 10.12809/hkmj134120
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
To scan or not to scan, to enhance or not to enhance? That is the question
Lily Li, MRCS (Eng), MB/BChir1; Jonathan Costello, MRCPI, FCEM2
1 Department of Trauma and Orthopaedics, Lister Hospital, Stevenage,
Hertfordshire SG1 4AB, United Kingdom
2 Emergency Department, Royal Free Hospital, London NW3 2QG, United
Kingdom
Corresponding author: Dr Lily Li (xl228@doctors.org.uk)
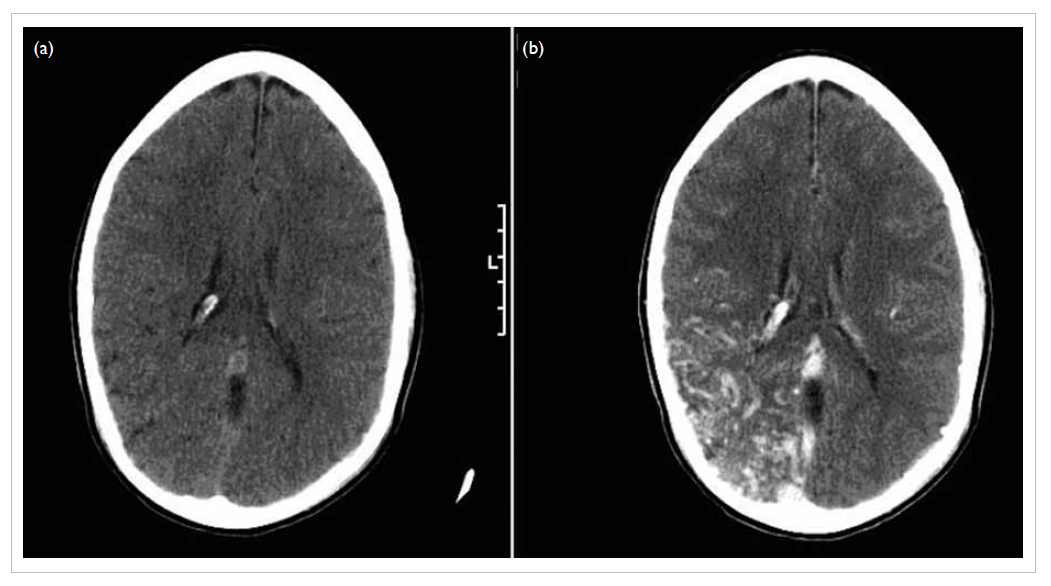
A 12-year-old boy presented to the Emergency
Department (ED) with reduced level of consciousness
in February 2011. Collateral history established a pre-hospital
witnessed seizure (requiring benzodiazepine
administration) preceded by auditory hallucinations.
Apart from uncomplicated malaria at the age of 5 years,
there was no other medical history of relevance. Initial
review was consistent with post-ictal presentation. An
additional generalised seizure was witnessed in the ED
within 30 minutes of admission requiring termination
with additional intravenous benzodiazepine. In
view of recurrent presentation, he was electively
intubated and commenced on parenteral phenytoin.
In addition, empirical acyclovir and ceftriaxone were
administered. An unenhanced computed tomographic
(CT) scan was normal (a). However, a subsequent
enhanced scan revealed diffuse right parieto-occipital
arteriovenous malformation (b). This case challenges
the prevalent practice of non-performance of CT in
new-onset seizure disorders and, if performed, the
practice of performing solely non-enhanced CT scans
in such presentations.