DOI: 10.12809/hkmj134097
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Recipes and general herbal formulae in books: causes of herbal poisoning
YK Chong, MB, BS1; CK Ching, FRCPA, FHKAM (Pathology)1; SW Ng, MPhil1; ML Tse, FHKCEM, FHKAM (Emergency Medicine)2; Tony WL Mak, FRCPath, FHKAM (Pathology)1
1 Hospital Authority Toxicology Reference Laboratory, Princess Margaret
Hospital, Laichikok, Hong Kong
2 Hong Kong Poison Information Centre, United Christian Hospital, Hospital Authority, Hong Kong
Corresponding author: Dr Tony WL Mak (makwl@ha.org.hk)
Abstract
Traditional Chinese medicine is commonly used
locally, not only for disease treatment but also for
improving health. Many people prepare soups
containing herbs or herbal decoctions according
to recipes and general herbal formulae commonly
available in books, magazines, and newspapers
without consulting Chinese medicine practitioners.
However, such practice can be dangerous. We report
five cases of poisoning from 2007 to 2012 occurring
as a result of inappropriate use of herbs in recipes
or general herbal formulae acquired from books.
Aconite poisoning due to overdose or inadequate
processing accounted for three cases. The other two
cases involved the use of herbs containing Strychnos
alkaloids and Sophora alkaloids. These cases
demonstrated that inappropriate use of Chinese medicine can result in major morbidity, and herbal
formulae and recipes containing herbs available in
general publications are not always safe.
Introduction
Traditional Chinese medicine (TCM) is generally
regarded by the public as benign and non-toxic
compared with western medications. However, this
belief may be untrue. Indeed, herbal poisoning cases
are not uncommon locally.1 2 Traditional Chinese
medicine is often considered by the Chinese as part of
a ‘healthy’ diet to improve the general health. Instead
of consulting Chinese medicine practitioners, many
people prepare herbal soups or decoctions according
to recipes and herbal formulae commonly available
in books, magazines, and newspapers. However, the
risk of such practice may be under-recognised.
From 2007 to 2012, the Hospital Authority
Toxicology Reference Laboratory confirmed five
cases of herbal poisoning related to the use of soups
or herbal decoctions prepared according to recipes
or general herbal formulae acquired from books. We
report these cases to highlight the potential danger
associated with such practice.
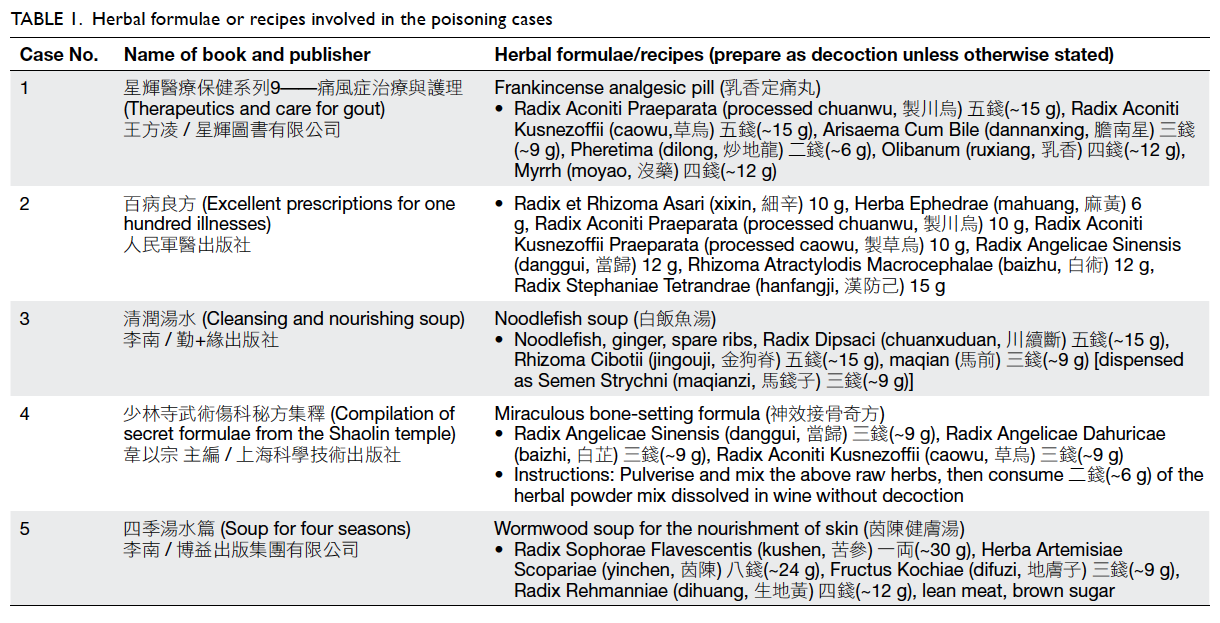
Case reports
Case 1
A 77-year-old man with a history of chronic
obstructive airway disease and gouty arthritis
presented in April 2008 with shortness of breath
and generalised numbness. His symptoms started
1 hour after consumption of a herbal decoction prepared from a formula “Frankincense analgesic
pill” available in the book “Therapeutics and care
for gout”. He developed atrial fibrillation and
hypotension, and later deteriorated into respiratory
failure necessitating intubation and ventilation with
intensive care. He also developed multiple episodes
of ventricular fibrillation. His condition improved
after supportive treatment, and he was discharged 5
days after admission.
Liquid chromatography–tandem mass
spectrometry (LC-MS/MS) of herbal remnants
and urine specimens showed presence of
Aconitum alkaloids (yunaconitine, hypoaconitine,
mesaconitine, aconitine). Thus, the patient was
diagnosed with severe aconite poisoning. The herbal
formula was found to contain two aconite herbs,
processed chuanwu 15 g and caowu 15 g, among
other herbs (Table 1). The dosages were 5 times
the upper limit of recommended dosages in the 2010
Chinese Pharmacopoeia,3 and worse still, it was not
mentioned whether caowu in the formula had been
processed (Table 2).
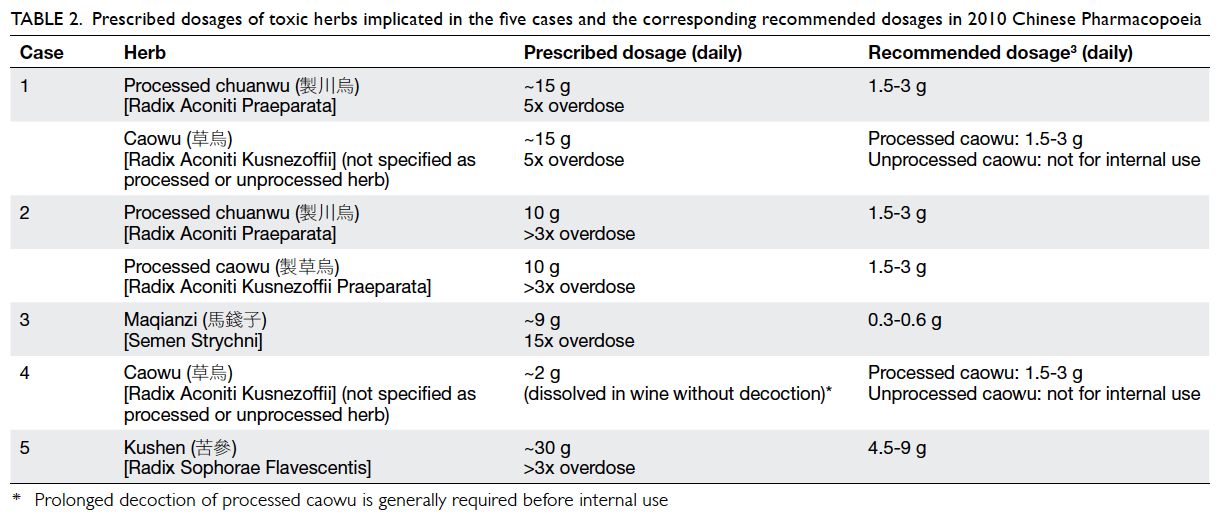
Table 2. Prescribed dosages of toxic herbs implicated in the five cases and the corresponding recommended dosages in 2010 Chinese Pharmacopoeia
Case 2
A 52-year-old man presented in March 2009 with
generalised numbness, weakness, and abdominal
pain after taking a herbal decoction prepared from
a formula in the book “Excellent prescriptions for
one hundred illnesses”. He complained of palpitation and was found to have ventricular bigeminy. He
developed shock shortly afterwards requiring
dopamine infusion. His condition improved with
supportive management and he was discharged after
3 days.
There were seven herbs in the formula, including
processed chuanwu 10 g and processed caowu
10 g (Table 1). Aconitum alkaloids (yunaconitine,
aconitine, deoxyaconitine, hypaconitine, and
mesaconitine) and their hydrolysed products were
detected in both urine and herbal remnant samples
by LC-MS/MS and gas chromatography–mass
spectrometry (GC-MS). The patient was diagnosed
with severe aconite poisoning. Contributory factors
included a three-fold overdose (Tables 1 and 2), and
the concomitant use of two aconite herbs.
Case 3
A 54-year-old woman presented in November
2007 with a 2-day history of leg cramps, dizziness,
sweating, and vomiting. She reported taking
“Noodlefish soup” for her knee pain based on a
recipe in the book “Cleansing and nourishing soup”.
She had doubled the doses of all ingredients. She
experienced mild leg cramping 2 hours after taking
the soup. She reboiled the soup and consumed two
doses on the next day; then, she developed bilateral
lower limb cramping, tonic contractions, dizziness,
nausea, and vomiting. The patient was discharged
after 1 day of observation.
In the urine and herbal broth specimens,
Strychnos alkaloids (strychnine and brucine) were
detected by GC-MS and high-performance liquid
chromatography with diode-array detector.
The clinical diagnosis was strychnine
poisoning. The recipe contained 9 g of “maqian”
(Table 1), which is a synonym of maqianzi.4 The
dosage was 15 times higher than the recommended
dosage (Table 2).
Case 4
A 66-year-old man, with multiple medical diseases,
presented in February 2012 with hypotension and
dizziness 1 hour after consumption of herbal powder
prepared according to a “Miraculous bone-setting
formula” available in the book “Compilation of secret
formulae from the Shaolin temple”. He required fluid
resuscitation and was discharged on the second day.
In the herbal powder and urine sample, Aconitum alkaloids (aconitine, mesaconitine,
hypaconitine, yunaconitine, and deoxyaconitine)
and their hydrolysed products were detected
by GC-MS and LC-MS/MS. The diagnosis was
moderate aconite poisoning. The formula was found
to contain caowu and two other herbs (Tables 1
and 2). According to the instruction, the patient
pulverised and mixed 9 g of each of the three herbs,
and then consumed 6 g of the mixed herbal powder
dissolved in wine without decoction. Although the
actual dose of caowu consumed (2 g) was within the
recommended dosage, the herb was not intended for
internal use before prolonged decoction to hydrolyse
the toxic Aconitum alkaloids.
Case 5
A 40-year-old woman presented in October 2009
with nausea, vomiting, dizziness, and sweating 50
minutes after taking a bowl of soup prepared from
a recipe “Wormwood soup for the nourishment of
skin” in the book “Soup for four seasons” for her
skin rash. The ingredients of the recipe included
kushen 30 g among other ingredients (Table 1).
Neurological examination was unremarkable.
Clinically, matrine poisoning was suspected. After 4
hours of observation, her symptoms improved and
she was discharged.
The herbal remnant and urine samples were
found to contain Sophora alkaloids (matrine,
sophoridine, cytisine, and N-methylcytisine) by
GC-MS. The diagnosis was matrine poisoning.
The dosage of kushen in the recipe was 3 times
higher than the upper limit of recommended dosage
(Table 2).3
Discussion
In the Chinese culture, medicine and food are
considered one inseparable entity. It is very common
for the Chinese to add medicinal herbs in their soups
and dishes to achieve different goals—prevention of
illness, treatment of disease, and nourishment of the
body. Rather than consulting a Chinese medicine
practitioner, it is not uncommon for the Chinese
to prepare herbal decoctions or soups according
to formulae or recipes in newspapers, magazines,
or books. The risk associated with such practice,
however, may be under-recognised, as illustrated by
our cases.
Three of the five cases (cases 1, 2, and 4)
reported here were related to the use of aconite herbs,
which are frequently used in TCM for their anti-inflammatory
and analgesic properties. However,
aconite herbs are toxic with low therapeutic indices,
and processing and prolonged decoction are
necessary before internal use. Aconite poisoning,
characterised by limb and perioral numbness,
arrhythmia, hypotension and gastro-intestinal
disturbances, is the most common cause of severe
herbal poisoning locally.5 Our group has previously
summarised the clinical features of 52 cases of
aconite poisoning.1 Concerning the three cases
reported here, overdose was the cause of poisoning
in two cases, whereas the use of herbs without prior
decoction accounted for poisoning in the third one.
The issue of overdosing is further illustrated by
case 5, in which overdose of kushen (3 times the
recommended dose) was identified as the cause of
matrine poisoning. Sophora alkaloids, present in the
herb kushen, are known to cause dizziness, nausea, and vomiting.6 Neurological toxicity has also been
reported in severe cases.
The cause of strychnine poisoning in case 3
was traced to a typesetting error in the book; the
text said “maqian” instead of “mati” (water chestnut).
This was confirmed by crosschecking with the same
recipe in another book by the same author. Severe
strychnine poisoning can cause muscle twitching,
convulsions, rhabdomyolysis, and even death.
Despite doubling the dose of all herbs in the soup
with a 15 times higher dose of maqianzi, the clinical
toxicity of the patient was relatively mild. It could be
related to the fact that maqianzi was not pulverised
and remained intact after boiling.
The chain of events leading to clinical poisoning
in these cases reflects failure of multiple parties in
practising safe use of Chinese herbs. The authors
should exercise careful judgement in choosing safe
herbal formulae or recipes for inclusion in their
books, and there should be adequate quality control
by editors, especially to prevent typographic errors
that can lead to grave consequences. The general
public should be educated that Chinese medicine is
not always benign and safe, and consulting a Chinese
medicine practitioner before taking herbs is always
advisable.
The fact that gross overdoses of herbs were
being dispensed from the herbal shops also played
a role in these poisoning cases. Currently, except
the Schedule 1 Chinese medicines, no guideline
exists in Hong Kong on the maximum dosage of
a particular herb, including the toxic processed
aconite herbs, above which one cannot dispense.
Of note, the dosages dispensed in these cases were
well above the dosage recommended in the Chinese
Pharmacopoeia.7 We believe that the availability of
such guidelines will serve to improve the safety of
TCM.
Awareness and knowledge of common herbal poisoning among clinicians can allow correct
diagnosis and timely treatment of the poisoned
patients. Laboratory analyses of the herbal samples
and biological samples can help to confirm the
diagnosis.
Conclusion
The five unfortunate cases in this series illustrate that
inappropriate use of Chinese medicine can result
in significant morbidity. General herbal formulae
and recipes containing herbs are not always safe.
Enhancing the standards of these publications,
improving the practice of dispensing herbs, and
public education on the safe use of Chinese medicine
will, hopefully, prevent similar cases from happening
again.
References
1. Chen SP, Ng SW, Poon WT, et al. Aconite poisoning over
5 years: a case series in Hong Kong and lessons towards
herbal safety. Drug Saf 2012;35:575-87. CrossRef
2. Cheng KL, Chan YC, Mak TW, Tse ML, Lau FL. Chinese
herbal medicine–induced anticholinergic poisoning in
Hong Kong. Hong Kong Med J 2013;19:38-41.
3. State Pharmacopoeia Commission. Chinese
Pharmacopoeia 2010. Volume I. Beijing, China: Chemical
Industry Press; 2010.
4. State Administration of Traditional Chinese Medicine; the
editorial committee of Chinese Materia Medica. China:
Shanghai Science and Technology Press; 1999.
5. Chan TY, Chan JC, Tomlinson B, Critchley JA. Chinese
herbal medicines revisited: a Hong Kong perspective.
Lancet 1993;342:1532-4. CrossRef
6. Drew AK, Bensoussan A, Whyte IM, Dawson AH, Zhu X,
Myers SP. Chinese herbal medicine toxicology database:
monograph on Radix Sophorae Flavescentis, “ku shen”. J
Toxicol Clin Toxicol 2002;40:173-6. CrossRef
7. Hong Kong Special Administrative Region Government.
Chinese Medicine Ordinance (Cap 549, Laws of Hong
Kong); 2010.