Hong Kong Med J 2014;20:264.e1–2 | Number 3, June 2014
DOI: 10.12809/hkmj133983
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
More than skin deep: Paget’s disease of the
perineum
JW Li, MB, BS, MRCP; CM Ng, MRCP, FHKAM
Department of Medicine, Queen Elizabeth
Hospital, 30 Gascoigne Road, Kowloon, Hong Kong
Corresponding author: Dr JW Li (lijohnwing@gmail.com)
In July 2012, an extensive eczematous
lesion was found incidentally over the external genitalia in a
77-year-old man who was being evaluated for lower limb cellulitis.
The affected area had been present for 10 years; it was
erythematous, macerated, and itchy. He had consulted countless
doctors, but the itchiness was intense and the area of involvement
was enlarging despite application of topical creams. On physical
examination, the perineum was weepy with excoriation, crusts, and
a serous discharge. The erythematous skin was indurated and had a
well-defined margin. The penis shaft was swollen with palpable
groin lymph nodes (Fig 1). Blood tests showed eosinophilia
(1.1 x 109/L) and an elevated erythrocyte sedimentation
rate (58 mm/h).

Figure 1. Clinical picture of extramammary Paget’s disease of the perineum, showing its weepy nature and the sharp margin around the affected area
A clinical suspicion of extramammary
Paget’s disease (EMPD) was suggested by the dermatologist. Skin
biopsy of the right suprapubic region confirmed the diagnosis (Fig 2), while another biopsy of the left
groin showed poorly differentiated invasive carcinoma, consistent
with invasive EMPD. Urine for cytology, as part of the malignancy
screening, showed atypical cells. Computed tomography of the
abdomen revealed left ureteric obstruction with enhanced mural
thickening of left ureter, of which transitional cell carcinoma
could not be excluded. He was referred to a urologist for further
assessment. Radiotherapy to the affected skin lesions was given in
view of the extensive involvement.
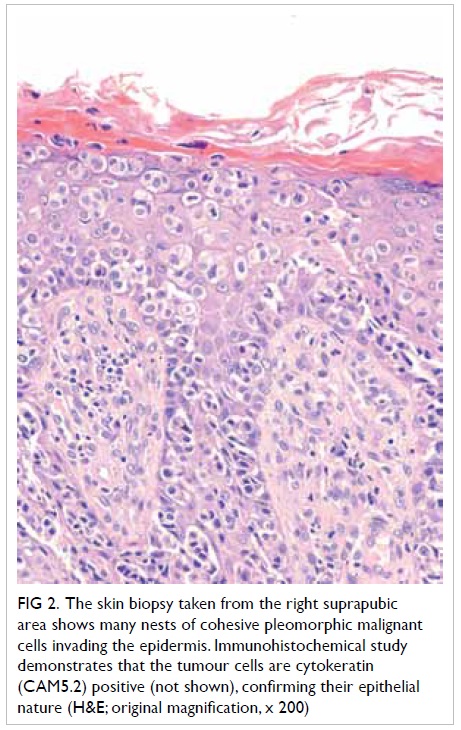
Figure 2. The skin biopsy taken from the right suprapubic area shows many nests of cohesive pleomorphic malignant cells invading the epidermis. Immunohistochemical study demonstrates that the tumour cells are cytokeratin (CAM5.2) positive (not shown), confirming their epithelial nature (H&E; original magnification, x 200)
Extramammary Paget’s disease is a rare
intraepithelial adenocarcinoma of the skin rich in apocrine
glands, first described by Crocker in 1888.1 The disease involves the epidermis, but can
potentially metastasise via the lymphatic system.2 Its clinical and histological features are
similar to Paget’s disease of the nipple. The penis, scrotum, and
vulva are frequently involved in sites. The erythematous area has
a sharp margin and scaly surface. Intense itchiness is common and
may result in erosion, excoriation, and lichenification.2
Our patient had a typical presentation with
longstanding, distressing, and difficult-to-treat, eczema-like
perineal lesion with a well-defined border. Delay in diagnosis, up
to a decade,3 is
notoriously common, because EMPD often mimics benign
dermatological diseases such as eczema, contact dermatitis and
fungal infection, and even malignant skin conditions like
superficial melanoma, basal cell carcinoma, and Bowen’s disease.
A clinical diagnosis should be confirmed by
skin biopsy. Immunohistochemistry shows the cells are positive for
CEA, CAM 5.2, as well as keratins CK7 and 8. Once EMPD is
diagnosed, thorough search for malignancy is mandatory, since up
to 37% of patients have associated malignancies, in which case the
condition is referred to as secondary EMPD.4 A recent study among Chinese patients showed
that 8.3% out of 48 patients with EMPD developed malignancy.3 Location of skin involvement in EMPD predicts
the type of cancer; perianal lesions are associated with anal and
colorectal cancer, whereas penoscrotal lesions tend to be
associated with urogenital malignancies.4
The positivity of Cytokeratin 20 in immunostaining is also highly
associated with internal malignancies.5
Treatment is mainly surgical resection with
reconstruction. Radiotherapy is an adjunctive therapy or reserved
for frail elderly patients.2
Photodynamic therapy and topical imiquimod have been used. Despite
these treatments, the local recurrence rate still ranges from 21%
to 61%,3 with a median time
to recurrence of 2 years.
Acknowledgement
We would like to thank Dr Shun-chin Ng,
Dermatologist, Department of Health, Hong Kong, for his clinical
care and manuscript advice. We thank Dr Wing-hung Lau, Department
of Pathology, Queen Elizabeth Hospital, for provision of
histological diagnosis and picture.
References
1. Crocker HR. Paget's disease
affecting the scrotum and penis. Trans Pathol Soc Lond
1888;40:187-91.
2. Burns T, Breathnach S, Cox N,
Griffiths C, editors. Rook's textbook of dermatology. 8th ed.
Oxford, UK: Wiley-Blackwell; 2010.
3. Chan JY, Li GK, Chung JH, Chow
VL. Extramammary Paget's disease: 20 years of experience in
Chinese population. Int J Surg Oncol 2012;2012:416418.
4. Sarmiento JM, Wolff BG, Burgart
LJ, Frizelle FA, Ilstrup DM. Paget's disease of the perianal
region—an aggressive disease? Dis Colon Rectum 1997;40:1187-94. CrossRef
5. Liegl B, Liegl S, Gogg-Kamerer
M, Tessaro B, Horn LC, Moinfar F. Mammary and extramammary Paget's
disease: an immunohistochemical study of 83 cases. Histopathology
2007;50:439-47. CrossRef

