Hong Kong Med J 2014;20:255–7 | Number 3, June 2014
DOI: 10.12809/hkmj133971
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Acute appendicitis complicating Amyand’s hernia: imaging features and literature review
WK Tsang, FRCR, FHKAM (Radiology)1;
KL Lee, FRCR, FHKAM (Radiology)2;
KF Tam, FRCR, FHKAM (Radiology)3;
SF Lee, FRCR, FHKAM (Radiology)3
1 Department of Radiology and Imaging, Queen Elizabeth Hospital, Hong
Kong
2 Department of Imaging and Interventional Radiology, Prince of Wales
Hospital, Shatin, Hong Kong
3 Department of Radiology, North District Hospital, Sheung Shui, Hong
Kong
Corresponding author: Dr WK Tsang (tsang_k@yahoo.com.hk)
Abstract
Acute appendicitis complicating Amyand’s hernia is
an extremely rare condition, in which the appendix
herniates into the inguinal sac and, subsequently,
gets inflamed. The condition is difficult to diagnose
clinically. Imaging is valuable for its diagnosis and
detection of the associated complications. In this
article, we will discuss the imaging features of acute
appendicitis complicating Amyand’s hernia and the
results of a literature review on the condition.
Introduction
Amyand’s hernia is a rare condition in which the
appendix herniates into the inguinal sac. It is most
commonly detected incidentally during hernia repair. Acute appendicitis in Amyand’s hernia occurs even
less frequently, and is difficult to diagnose clinically.
Imaging is valuable for its diagnosis and detection
of the associated complications. Here we report
our experience with this disease entity, its imaging
features, and the results of a literature review.
Case report
An 82-year-old man with unremarkable history
presented to the surgeons with fever and generalised
abdominal pain. On physical examination, he had a
temperature of 38.8°C, diffuse abdominal tenderness,
and a tender, irreducible right inguinal lump.
Laboratory tests revealed mildly elevated white
cell count. His supine abdominal radiography was
unremarkable. A provisional diagnosis of irreducible
right inguinal hernia was made. However, it was
atypical that the patient did not have symptoms or
signs suggestive of intestinal obstruction. Urgent
ultrasonography (USG) of the right groin showed a
blind-ending fluid-filled tubular structure within the
right scrotal sac. This structure extended superiorly
along the inguinal canal, entered the right lower
abdomen and joined the caecum (Fig 1a). It was
compatible with the appendix. Acute inflammation
was indicated by wall hypervascularity and tenderness
elicited upon compression. There was no
adjacent free fluid or collection to suggest abscess
formation or a ruptured appendix. The diagnosis
was confirmed by computed tomography (CT)
as dilated appendix with wall hyperenhancement
and herniation into the right scrotal sac (Fig 1b).
Periappendiceal strandings, reactive regional lymph
nodes, and oedematous right scrotal wall were noted. Emergency appendectomy and right inguinal
herniorrhaphy were performed. A pus-filled
appendix was revealed within the right scrotal sac
during the procedure (Fig 2).
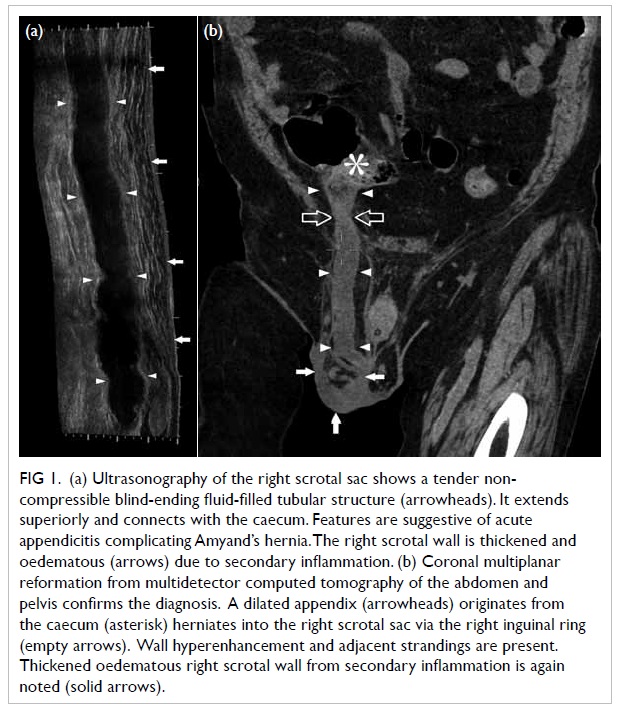
Figure 1. (a) Ultrasonography of the right scrotal sac shows a tender noncompressible blind-ending fluid-filled tubular structure (arrowheads). It extends superiorly and connects with the caecum. Features are suggestive of acute appendicitis complicating Amyand’s hernia. The right scrotal wall is thickened and oedematous (arrows) due to secondary inflammation. (b) Coronal multiplanar reformation from multidetector computed tomography of the abdomen and pelvis confirms the diagnosis. A dilated appendix (arrowheads) originates from the caecum (asterisk) herniates into the right scrotal sac via the right inguinal ring (empty arrows). Wall hyperenhancement and adjacent strandings are present. Thickened oedematous right scrotal wall from secondary inflammation is again noted (solid arrows)
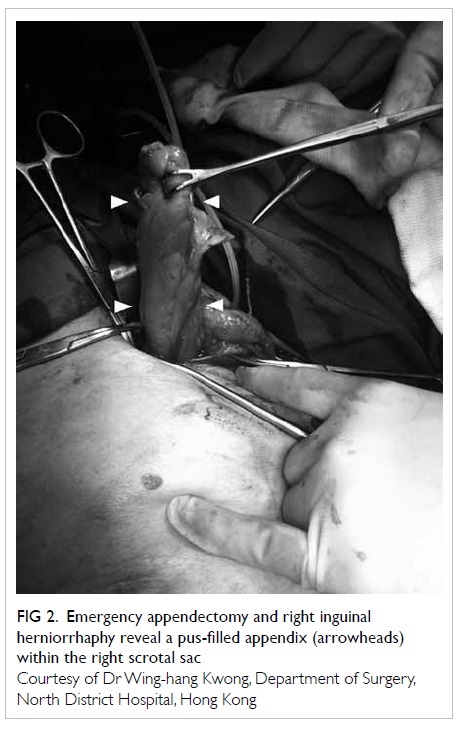
Figure 2. Emergency appendectomy and right inguinal herniorrhaphy reveal a pus-filled appendix (arrowheads) within the right scrotal sac
Discussion
Amyand’s hernia is named after Claudius Amyand
(1660-1735), a sergeant-surgeon to King George II of
England. In 1735, he performed the first documented
successful appendectomy on an 11-year-old boy who
had a perforated, acutely inflamed appendix within
the right scrotal sac.1 The appendix was perforated
by a previously swallowed pin, leading to formation
of an enterocutaneous fistula.
Amyand’s hernia is uncommon, with a
prevalence of 1% among all the repaired inguinal
hernias.2 Most often, it is found incidentally during
surgery.2 It is more frequent in males. The condition
may present in individuals from any age, through
premature neonates to the elderly people.3 4 The
majority of cases occur on the right side, the side
where appendix normally locates and inguinal hernia
more commonly happens. Less than 10 cases of
left-sided Amyand’s hernia have been reported in
the literature; these can occur in patients with situs
inversus, intestinal malrotation, or a mobile caecum.5 6 7 8 9
Appendicitis more frequently occurs in
Amyand’s hernia than in appendix at normal
position. The superficial location of the appendix
within the inguinal sac can possibly make it more
vulnerable to trauma and secondary inflammation.
Another postulation is that the abdominal muscles
can constrict the hernial orifice and induce
intermittent compression of the appendix. This might
induce ischaemia of the appendix and make it more
susceptible to infection.10 Apart from appendicitis,
the other documented complications of Amyand’s
hernia include irreducibility and strangulation of
the appendix, abscess formation, peritonitis, and
enterocutaneous fistula formation.1 Other intra-abdominal
structures such as the caecum, urinary
bladder, and omentum can accompany the appendix
and herniate into the hernial sac.6 7
The diagnosis of Amyand’s hernia is rarely
made clinically. Most often it is mistaken as an
irreducible inguinal hernia. Imaging is valuable
for preoperative diagnosis and detection of any
complications. Coronal multiplanar reformations
from multidetector CT of the abdomen and pelvis
are excellent imaging modalities for demonstrating
a blind-ending tubular structure arising from the
caecum which extends into the inguinal sac. Luminal
dilatation, wall thickening and hyperenhancement,
adjacent stranding and fluid are suggestive of acute
appendicitis. Complications such as perforation and
abscess formation should be sought. In children and
pregnant women, USG and magnetic resonance
imaging are preferred with the advantage of being
radiation free. In USG, the acutely inflamed
appendix appears dilated, non-compressible with
thickened hypervascular wall, and is tender upon
compression.11 12 Sometimes the connection between
the appendix and caecum might not be readily
demonstrable, especially in overweight and pregnant
patients.
The differentiation between usual inguinal
hernias and Amyand’s hernia can be readily made
by imaging. In usual inguinal hernia, a segment of
small or large bowel is seen within the hernial sac.
Littre’s hernia, which is defined as herniation of
Meckel’s diverticulum, can mimic Amyand’s hernia
both clinically and radiologically. It occurs in 11% of patients with Meckel’s diverticulum. Similar to
Amyand’s hernia, Littre’s hernia is more prevalent in
males and on the right side.13 About 50% of the cases
occur in the inguinal region, with 20% occurring
in the femoral canal, and 20% in the umbilicus.14
Just like Amyand’s hernia, a blind-ending tubular
structure can be found in Littre’s hernia. Instead
of arising from the caecum, it originates from the
antimesenteric border of the distal small bowel.15
In addition, a normal appendix should be detected
in patients with Littre’s hernia unless it has been
resected.
Conclusion
Acute appendicitis complicating Amyand’s hernia is
extremely rare and is difficult to diagnose clinically.
Imaging is valuable for its diagnosis and detection of
associated complications.
References
1. Amyand C. Of an inguinal rupture, with a pin in the appendix caeci, incrusted with stone; and some observations on wounds in the guts. Phil Trans R Soc Lond 1736;39:329-36. CrossRef
2. Psarras K, Lalountas M, Baltatzis M, et al. Amyand's hernia—a vermiform appendix presenting in an inguinal hernia: a case series. J Med Case Rep 2011;5:463. CrossRef
3. Livaditi E, Mavridis G, Christopoulos-Geroulanos G. Amyand's hernia in premature neonates: report of two cases. Hernia 2007;11:547-9. CrossRef
4. Yang W, Tao Z, Chen H, et al. Amyand's hernia in elderly patients: diagnostic, anesthetic, and perioperative considerations. J Invest Surg 2009;22:426-9. CrossRef
5. Bakhshi GD, Bhandarwar AH, Govila AA. Acute appendicitis in left scrotum. Indian J Gastroenterol 2004;23:195.
6. Ghafouri A, Anbara T, Foroutankia R. A rare case report of appendix and cecum in the sac of left inguinal hernia (left Amyand's hernia). Med J Islam Repub Iran 2012;26:94-5.
7. Ravishankaran P, Mohan G, Srinivasan A, Ravindran G, Ramalingam A. Left sided Amyand's hernia, a rare occurrence: a case report. Indian J Surg 2013;75:247-8. CrossRef
8. Khan RA, Wahab S, Ghani I. Left-sided strangulated Amyand's hernia presenting as testicular torsion in an infant. Hernia 2011;15:83-4. CrossRef
9. Singh K, Singh RR, Kaur S. Amyand's hernia. J Indian Assoc Pediatr Surg 2011;16:171-2. CrossRef
10. Abu-Dalu J, Urca I. Incarcerated inguinal hernia with a perforated appendix and periappendicular abscess: report of a case. Dis Colon Rectum 1972;15:464-5. CrossRef
11. Akfirat M, Kazez A, Serhatlioğlu S. Preoperative sonographic diagnosis of sliding appendiceal inguinal hernia. J Clin Ultrasound 1999;27:156-8. CrossRef
12. Celik A, Ergün O, Ozbek SS, Dökümcü Z, Balik E. Sliding appendiceal inguinal hernia: preoperative sonographic diagnosis. J Clin Ultrasound 2003;31:156-8. CrossRef
13. Shahid N, Ibrahim K. Littre's hernia. Professional Med J 2005;12:479-81.
14. Fa-Si-Oen PR, Roumen RM, Croiset van Uchelen FA. Complications and management of Meckel’s diverticulum: a review. Eur J Surg 1999;165:674-8. CrossRef
15. Sinha R. Bowel obstruction due to Littre hernia: CT diagnosis. Abdom Imaging 2005;30:682-4. CrossRef

