Hong Kong Med J 2014;20:168.e1–2 | Number 2, April 2014
DOI: 10.12809/hkmj133844
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
A rare cause of haematochezia: pyogenic granuloma in colon
KL Lui, MRCP(UK), FHKCP1;
KS Ng, MB, ChB2; Michael KK Li, FRCP, FHKAM (Medicine)1
1 Division of Gastroenterology and Hepatology, Department of Medicine
and Geriatrics, Tuen Mun Hospital, Tuen Mun, Hong Kong
2 Department of Pathology, Tuen Mun Hospital, Tuen Mun, Hong Kong
Corresponding author: Dr MKK Li (klluitc@yahoo.com.hk)
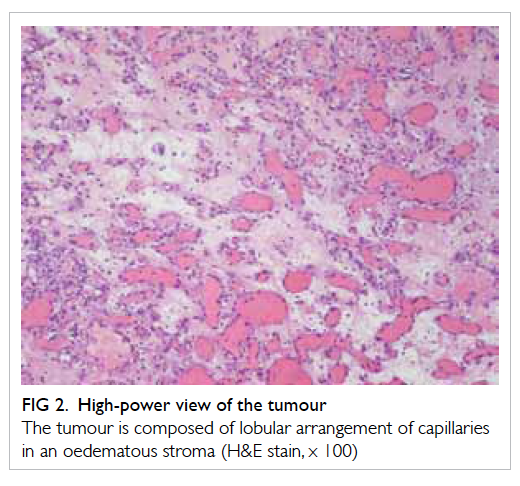
A 74-year-old man presented with haematochezia
(passage of fresh blood per rectum) for 1 day, and
a history of diabetic nephropathy and fatty liver
going back 10 years. The haemoglobin level dropped
from 140 g/L to 90 g/L over 6 months. Colonoscopy
revealed a ‘malignant looking’ ascending colon polyp
with a whitish coating and easy contact bleeding (Fig 1). Polypectomy was performed but complicated
with profuse bleeding which was controlled with a
haemoclip. The histology confirmed the lesion to be
pyogenic granuloma (PG) with a lobular arrangement
of capillaries in an oedematous stroma (Fig 2) and
endothelial cells staining positive for CD31, CD34 (Fig 3), and tissue factor VIII.
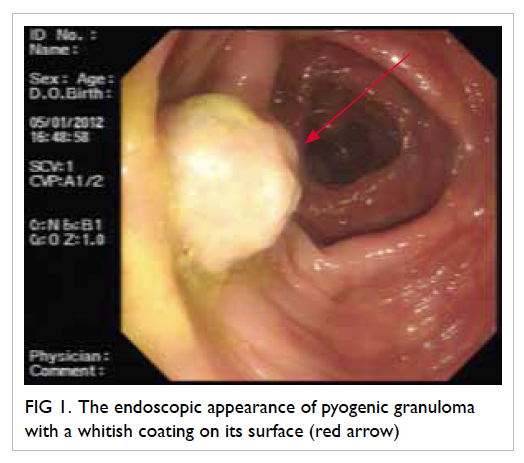
Figure 1. The endoscopic appearance of pyogenic granuloma with a whitish coating on its surface (red arrow)
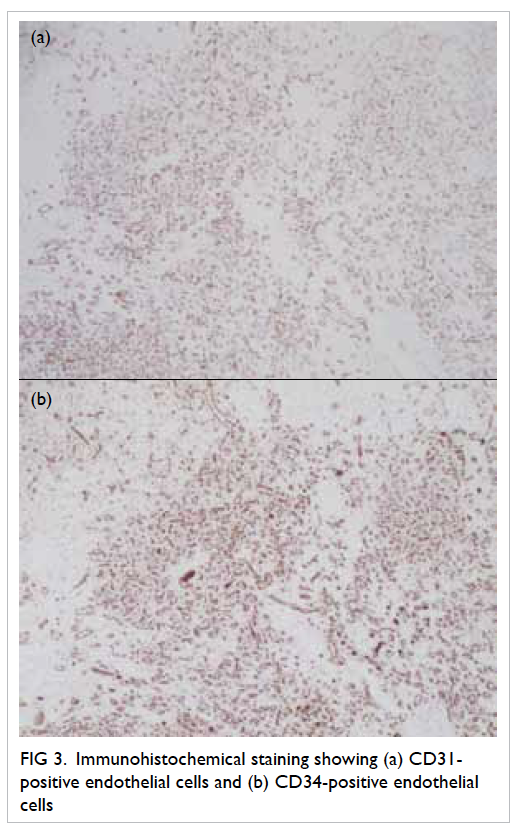
Figure 3. Immunohistochemical staining showing (a) CD31-positive endothelial cells and (b) CD34-positive endothelial cells
This form of granuloma is a very rare cause of
haematochezia. Usually, PG occurs on the skin after
repeated trauma; only a few colonic cases have been
reported.1 2 Macroscopically, it is usually described as
a red, polypoid mass of apparent granulation tissue
and surface ulceration or with a whitish coating that
bleeds easily upon contact. Microscopically it is best
described as a capillary haemangioma arranged in
a lobular pattern, with clusters of small capillaries
lined by a single layer of bland endothelial cells. The
stroma is often oedematous and filled with a dense
neutrophilic infiltrate. The most useful markers are
the presence of elements that stain for tissue factors
VIII and CD31, and CD34, on endothelial cells
lining capillary loops. The exact cause of PG remains
unknown, but trauma, post-irritation, post-surgery,
viral causes (eg human herpesvirus–8) have all been postulated but never proven.1 2 Colonic PGs usually
present with haematochezia with or without anaemia
and sometimes the bleeding can be massive. The
lesion is usually completely excised by endoscopic
polypectomy. However, since it bleeds extremely
easily, post-polypectomy haemostasis is usually
necessary and sometimes angiographic embolisation
is performed.3 Therefore, early recognition of the
endoscopic appearance of PGs is essential.
References
1. Iwasaka C, Yazu T, Suehiro A, et al. A case of pyogenic granuloma in the sigmoid colon [in Japanese]. Nippon Shokakibyo Gakkai Zasshi 1995;92:885-8.
2. Nakaya T, Tokunaga T, Aono S, et al. Pyogenic granuloma of the descending colon. Endoscopy 2007;39(Suppl 1):E259-60. CrossRef
3. Kusakabe A, Kato H, Hayashi K, et al. Pyogenic granuloma of the stomach successfully treated by endoscopic resection after transarterial embolization of the feeding artery. J Gastroenterol 2005;40:530-5. CrossRef