Hong Kong Med J 2014;20:126–33 | Number 2, April 2014 | Epub 14 Mar 2014
DOI: 10.12809/hkmj134076
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Public knowledge and attitudes towards cardiopulmonary resuscitation in Hong Kong: telephone survey
SY Chair, PhD1;
Maria SY Hung, DHSc, MN2;
Joseph CZ Lui, FHKCA, FHKAM (Anaesthesiology)3;
Diana TF Lee, PhD1;
Irene YC Shiu, MHA, MNurs (AdvPrac)4;
KC Choi, PhD1
1 The Nethersole School of Nursing, The Chinese University of Hong
Kong, Shatin, Hong Kong
2 School of Nursing, The Hong Kong Polytechnic University, Hunghom,
Hong Kong
3 United Christian Hospital, Hospital Authority, Hong Kong
4 Resuscitation Training Centre, Caritas Medical Centre, Shamshuipo,
Hong Kong
Corresponding author: Dr MSY Hung (maria.hung@polyu.edu.hk)
Abstract
Objectives: To investigate the public’s knowledge
and attitudes about cardiopulmonary resuscitation
in Hong Kong.
Design: Cross-sectional telephone survey.
Setting: Hong Kong.
Participants: Hong Kong residents aged 15 to 64
years.
Main outcome measures: The knowledge and
attitudes towards cardiopulmonary resuscitation.
Results: Among the 1013 respondents, only 214 (21%)
reported that they had received cardiopulmonary
resuscitation training. The majority (72%) of these
trained respondents had had their latest training
more than 2 years earlier. The main reasons for not
being involved in cardiopulmonary resuscitation
training included lack of time or interest, and “not
necessary”. People with full-time jobs and higher
levels of education were more likely to have such
training. Respondents stating they had received
cardiopulmonary resuscitation training were more
willing to try it if needed at home (odds ratio=3.3;
95% confidence interval, 2.4-4.6; P<0.001) and on
strangers in the street (4.3; 3.1-6.1; P<0.001) in case of
emergencies. Overall cardiopulmonary resuscitation
knowledge of the respondents was low (median=1,
out of 8). Among all the respondents, only four of them (0.4%) answered all the questions correctly.
Conclusions: Knowledge of cardiopulmonary
resuscitation was still poor among the public in
Hong Kong and the percentage of population
trained to perform it was also relatively low. Efforts
are needed to promote educational activities and
explore other approaches to skill reinforcement
and refreshment. Besides, we suggest enacting laws
to protect bystanders who offer cardiopulmonary
resuscitation, and incorporation of relevant training
course into secondary school and college curricula.
New knowledge added by this
study
- Knowledge of cardiopulmonary resuscitation (CPR) is still poor among members of the Hong Kong public, and a relatively low percentage of the population has received relevant training.
- The Hong Kong government and non-government organisations need to promote educational activities and explore other approaches to reinforce and refresh participation in CPR.
- There is a need to enact laws to increase public awareness of CPR and protect bystanders who perform it.
- Incorporating CPR training into the secondary schools and colleges as part of a general education course is warranted.
Introduction
Out-of-hospital cardiac arrest is a public health
problem and leads to the highest proportion of
deaths in many parts of the world.1 2 According
to the American Heart Association (AHA), in the
US and Canada, approximately 350 000 people
per year suffer out-of-hospital cardiac arrests for
which cardiopulmonary resuscitation (CPR) is
attempted.1 3 4 In Hong Kong, although no such
direct epidemiological information can be referred to, more than 1000 persons are believed to die
suddenly and unexpectedly each year; many of which
are presumed to be primarily due to cardiac arrests.5
For those who endure sudden cardiac arrests,
early, high-quality CPR can greatly improve chances
of survival.6 7 Nowadays, the importance of CPR is
well recognised and emphasised. Accordingly, the
AHA even recommended that CPR training and
familiarisation with automated external defibrillators
(AEDs) should be included in secondary school curricula.8 Thus, equipping the public with such skills
becomes one of the essential strategies to increase
the success of CPR for cardiac arrest victims.
In recent years, studies have been conducted
to examine the knowledge and attitude of the
public regarding CPR. In general, people had poor
knowledge on this subject and the proportion of
the public who had received the CPR training was
low.9 10 11 12 Besides, many individuals did not want to
perform cardiac compression with mouth-to-mouth
ventilation, due to fear of acquiring transmitted
diseases.13 These factors are likely to limit the numbers
of bystander CPRs carried out and contribute to
the low survival rates from out-of-hospital cardiac
arrests. A local study showed that for out-of-hospital
cardiac arrests, the frequency of bystander CPR was
only about 15.7% and the survival rate to eventual
discharge from hospital was as low as 1.3% in Hong
Kong.10
To identify effective measures to promote
CPR, the current situation should be evaluated.
This study aimed to explore the Hong Kong public’s
knowledge and attitudes about CPR. Its findings
could inform the community regarding preferences
to perform bystander CPR and more importantly it
could indicate directions for future training.
Methods
Population and data collection
This was a cross-sectional population-based survey. The study population comprised the
Chinese Hong Kong residents aged 15 to 64 years,
who speak Cantonese in domestic households.
Anonymous telephone interviews using a structured
questionnaire were conducted and launched in the
Telephone Survey Research Laboratory of the Hong
Kong Institute of Asia-Pacific Studies of The Chinese
University of Hong Kong. By using the Computer
Assisted Telephone Interviewing system, telephone
numbers were randomly selected from up-to-date
residential telephone directories that covered over
95% of Hong Kong households. The interviews were
conducted between 6:15 pm and 10:15 pm, to avoid
over-representing the non-working population. For
households with more than one eligible member,
the one whose birthday was closest to the interview
date was invited to join the study. At least three
attempts were made to contact individuals in any
given household. Such attempts were made at
different times of the day and/or different days
of the week, to avoid being labelled a non-contact
status (with an assigned number) so as to ensure
that survey results were not biased due to high non-contact/non-response rates. Eligible respondents
were briefed about the study and verbal consent
was sought. The study was approved by the Survey
and Behavioural Research Ethics Committee of The
Chinese University of Hong Kong.
Sample size
According to a previous study,11 12% of the population
had received CPR training. Owing to continuing
efforts and CPR promotion programmes/campaigns
by different associations and organisations in recent
years, it was expected that around 20% of the study
population had probably received prior CPR training.
Depending on the possible prevalence of subjects
with prior CPR training (ranging from 18 to 22%),
it was estimated that 883 to 1025 subjects would be
sufficient to estimate knowledge and attitudes with a
margin of error of ± 2.5% at 5% level of significance.
The sample size calculation was performed using
PASS 11 (NCSS, Kaysville [UT], US). Thus, we aimed
to recruit over 1000 subjects for this study.
Questionnaire
In this study we used a structured questionnaire,
which took about 5 to 10 minutes to complete, and was
developed in January 2010 (Appendix). It was based
on the 2005 AHA Guidelines for CPR and Emergency
Cardiovascular Care,14 Basic Life Support for
health care providers,15 and a review of the relevant
literature.11 12 It consisted of three sections. The first
entailed questions on demographics, including age,
gender, education level, occupation, family history
of heart disease, and ischaemic heart disease risk
factors. The second entailed questions about previous
CPR training. The third entailed questions on attitudes and knowledge regarding CPR. To evaluate
respondents’ relevant attitudes and knowledge,
questions were included about: willingness to
perform CPR (2 items), the basic knowledge related
to a victim’s response (1 item), management of
airway (2 items), breathing (2 items), circulation
(2 items), and AED usage (1 item). The anticipated
answers for the CPR knowledge questions (victim’s
response, management of airway, breathing, and
circulation) were consistent with information in
the latest AHA guidelines (2005 version). Content
validity was established by an expert panel including
four doctors and six nurses who were either AHA
Basic Life Support providers or instructors. The
content validity index rating item’s relevance to the
underlying construct was 0.96.
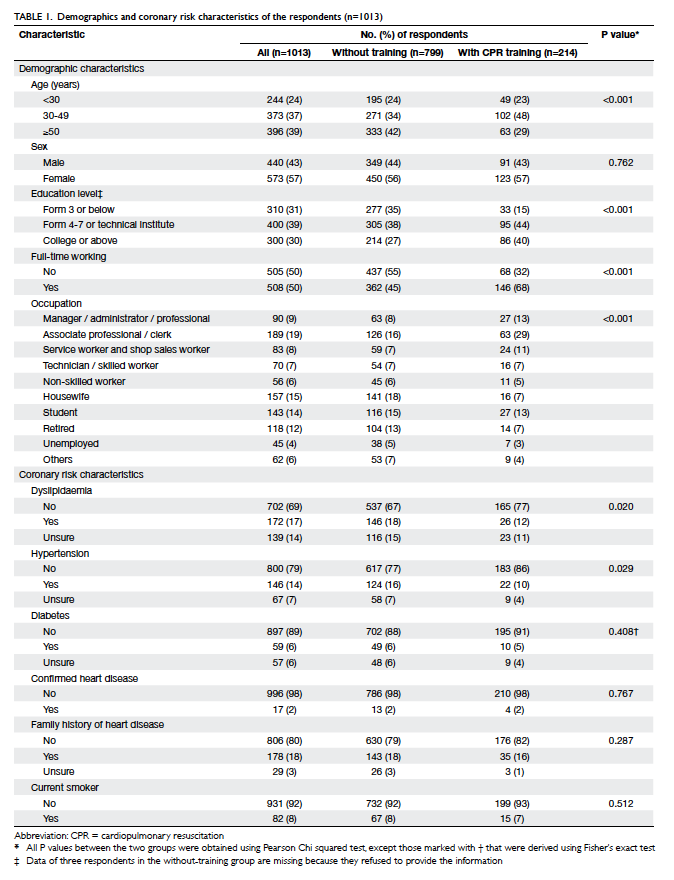
Statistical analyses
Data were categorised and presented in frequencies
(percentages). Univariate comparisons on
demographics and ischaemic heart disease risk
factors among those with and without CPR training
were conducted, using Pearson Chi squared or
Fisher’s exact tests, as appropriate. Logistic regression
analysis was used to identify demographics and
ischaemic heart disease risk factors (Table 1) that
were associated with CPR training. Variables
with a P value of <0.25 in the univariate analysis
were selected for use in the stepwise multivariate
logistic regression analysis, to delineate factors
independently associated with CPR training.16
Logistic regression models were also employed
to compare subjects with and without CPR training
with respect to various outcome variables (attitude
and knowledge about CPR), after adjustment for
demographics and coronary heart disease risk
factors. A ‘two-block stepwise’ logistic regression
modelling approach was used to make adjusted
comparisons of the two groups. The grouping factor
(CPR training: Yes/No) was first entered into logistic
regression model and then the demographics and
ischaemic heart disease risk factors (Table 1) were
entered in another block with stepwise selection.
In the final model, the adjusted odds ratio (OR)
to compare those with and without CPR training
(reference group) was derived, taking account of
demographics and ischaemic heart disease risk
factors. All statistical analyses were conducted using
SPSS 19.0 (Windows version 19.0; SPSS Inc, Chicago
[IL], US) with two-sided tests; a P value of <0.05 was
considered statistically significant.
Results
In this study, 2703 phone calls were not picked up
after three attempts, and 5669 calls were picked
up but 2735 calls were disconnected immediately
after knowing the purpose of the calls. A total of
2188 eligible respondents were identified, 1175 refused to participate. Finally, 1013 interviews were
conducted (response rate, 46%). The demographics
and ischaemic heart disease risk factors of these
respondents are shown in Table 1.
Cardiopulmonary resuscitation training
characteristics
Among the 1013 respondents, only 214 (21%)
reported that they had received CPR training;
the majority (72%, n=154) of whom had had their
latest training more than 2 years earlier. A large
proportion (63%, n=134) of the trained respondents
received their training via the Hong Kong St John
Ambulance (49%, n=104) and the Hong Kong Red
Cross (14%, n=30). Another 35 (16%) participants
had their training via their companies or workplaces. Their main reasons for taking CPR training
were ‘job requirement’ (48%, n=102) and ‘personal
interest’ (42%, n=90). For those who did not take
CPR training (n=799), most of them (74%, n=589)
claimed that they would not consider participating
in CPR training in the future. Reasons for not taking
CPR training could be multiple, and included ‘no
time’ (41%, n=241), ‘not necessary’ (26%, n=156), and
‘not interested’ (19%, n=110). In addition, 104 (18%)
participants picked ‘unable to learn CPR because of
their low education level or being too old’.
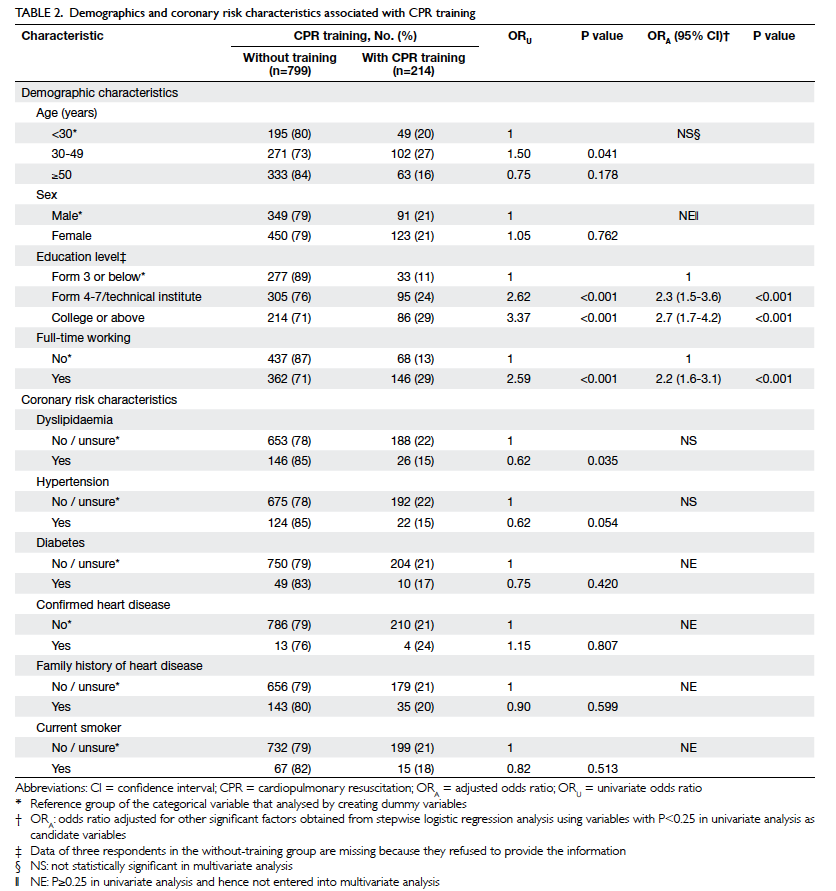
Factors associated with having
cardiopulmonary resuscitation training
Demographic and ischaemic heart disease risk
factors listed in Table 1 with a P value of <0.25 in
the univariate analysis were selected as candidate
variables for multivariate stepwise logistic
regression.16 Among them, age, education level,
full-time working status, occupation, having
dyslipidaemia and hypertension were associated
with having CPR training in the univariate analysis.
However, only having a full-time job (OR=2.2; 95%
confidence interval [CI], 1.6-3.1; P<0.001), middle
level education—Form 4-7/technical institute
(OR=2.3; 95% CI, 1.5-3.6; P<0.001), and a high level
of education—college or higher (OR=2.7; 95% CI,
1.7-4.2; P<0.001), were significantly associated with
having CPR training in the multivariate analysis.
Notably, having a low education level—Form 3 or
below—was not significantly associated with such
training (Table 2).
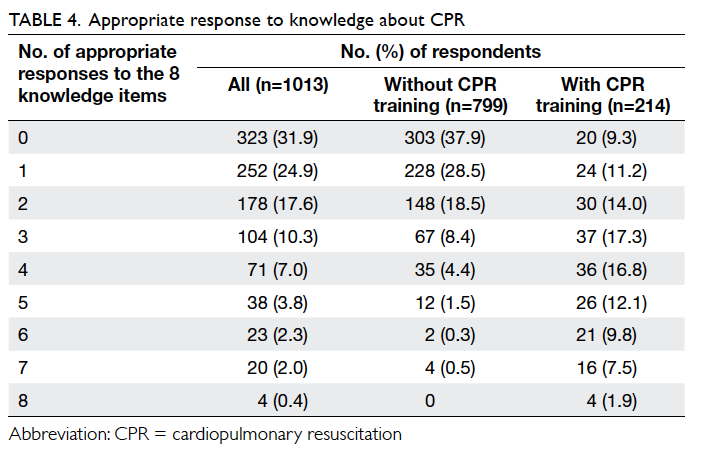
Willingness to perform cardiopulmonary
resuscitation
As shown in Table 3, the ratio of respondents with
and without training willing to attempt CPR on family
members at home was 72% vs 45% (P<0.001) and on
strangers in the street was 42% vs 15% (P<0.001).
Logistic regression analysis revealed that after
adjusting for potentially confounding demographic
and ischaemic heart disease risk factors, those with CPR training were also more likely to attempt CPR
at home (OR=3.3; 95% CI, 2.4-4.6; P<0.001) and
in the street (OR=4.3; 95% CI, 3.1-6.1; P<0.001) in
emergencies (Table 3).
Knowledge on cardiopulmonary
resuscitation
Regarding knowledge on CPR, trained respondents were more likely to give correct responses to each
of the eight knowledge questions (all P<0.001). After
adjusting for potential confounding demographic
and ischaemic heart disease risk factors, logistic
regression showed that the trained group was
significantly more likely to give five or more
appropriate responses to the eight knowledge items
when compared with those without such training (OR=19.8; 95% CI, 11.4-34.4; P<0.001; Table 3).
Although the trained respondents achieved higher
scores on CPR knowledge (median=3) than those
who were untrained (median=1), the overall
CPR knowledge level of the respondents was low
(median=1). Among all the 1013 respondents, only
four (0.4%) answered all the questions correctly
(score=8), which also represented 1.9% of those who
had received CPR training (Table 4).
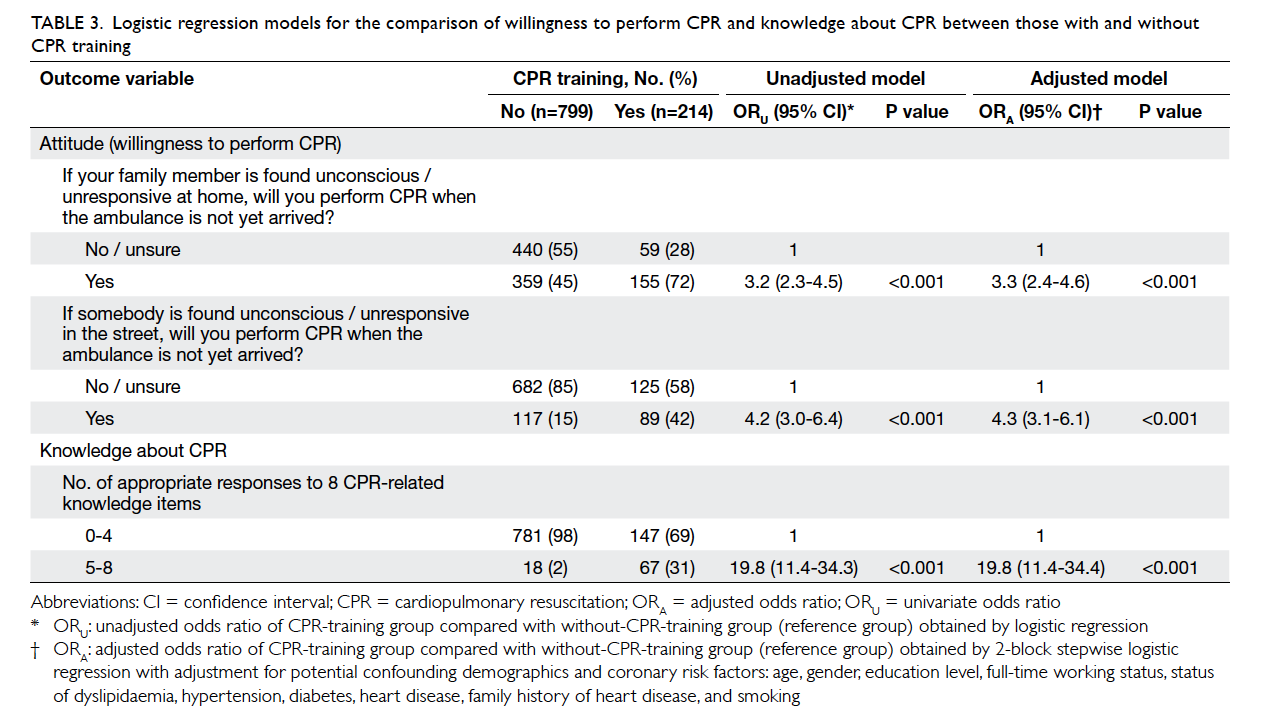
Table 3. Logistic regression models for the comparison of willingness to perform CPR and knowledge about CPR between those with and without CPR training
Discussion
The present study showed that 21% of the respondents had received CPR training, which was higher than in
a previous local study reporting 12%.11 Our rate was
comparable to data reported from elsewhere (27%
in New Zealand and 28% in Ireland),17 18 but much
lower than in reports from Australia (58%),19 Poland
(75%),20 and Washington (79%).21 Therefore, though
the trend for CPR training in Hong Kong seems to
be increasing, it seems far from sufficient, and the
majority had received their training more than 2
years earlier. Although it is commonly believed that
performing CPR without 100% accuracy is better
than doing nothing, whether our respondents could
perform appropriate CPR in an emergency was
questionable. In our cohort, skills appeared to have
deteriorated with time. One study suggested that
6-monthly reinstruction was needed to maintain
adequate CPR skills22; the 2-year intervals noted
in this study were much longer than what has
been suggested. Thus, after their first training, it is
suggested that individuals should attend refresher
courses. Moreover, the training institutions should pay more attention to remind the trainees on
the need for such reinstruction and updates.
The main reasons of taking CPR training were
“job requirement” and “personal interest”, which
were similar to reasons given in a previous study
from Ireland.18 Therefore, the workplace might
be considered a preferred place to conduct CPR
training in conjunction with government and non-government
organisations; in Hong Kong, these include St John Ambulance, the Hong Kong Red
Cross, and the Auxiliary Medical Services. In fact,
promoting CPR training in workplace seems an
important strategy, as 16% of trained respondents in
this study had already received such training in their
workplaces, and this was also in line with the results
of a study by Jennings et al.18
In this study, most non-trained respondents
would not consider receiving CPR training, giving
the following reasons: “no time”, “not necessary”, or
“not interested”. Lack of time for CPR training is a
common reason reported in different studies.11 23 24
To address this problem, self-instruction, such as via
video or internet training, may be considered. Studies
have shown that video self-instruction training
was as good as traditional classroom training,25 26
which is not only cost-effective but also flexible
compared to formal classroom training. In addition,
as recommended by the AHA,8 CPR training could
be incorporated into general education in secondary
schools. Several studies have investigated knowledge
and attitude towards CPR training, its feasibility
and the impact of CPR or life-supporting first-aid
training in primary and secondary schools in various
countries (Austria, Japan, and Norway) and reported
a positive experience.27 28 29 Either as part of the regular
curriculum, as mandatory courses, or as an elective
extra-curricular activity, it could be beneficial to
the students and the general public. By providing
students with CPR training, the first part of the chain
of survival in out-of-hospital cardiac arrest could
be enhanced for future generations, and increase
survival after sudden cardiac arrest. To successfully
carry out such a health and education policy, the
Hong Kong SAR Government can learn from other
Asian countries like Japan and Singapore, which
have already gained experience in CPR education for
secondary schools.
Those with full-time jobs and with higher levels
of education were more likely to attend CPR training,
which corresponded with the results of previous
studies.11 18 Not surprisingly 48% of respondents
in the present study were required to attend their
CPR training in connection with their jobs, while
18% believed that they were unable to learn as they
were too old or their level of education was too low.
Accordingly, this misunderstanding about CPR
needs correcting, and certainly CPR training should
be made available to those who are not employed.
Community centres could be used as possible
teaching venues to promote CPR, in conjunction
with the Hong Kong SAR Government and other
health care organisations (Hospital Authority, Hong
Kong Red Cross, and St John Ambulance). These
health-related organisations could play critical roles
in publicising the importance of CPR, and provide
accessible trainings for the public. Encouragingly, the Resuscitation Council of Hong Kong was established in 2012, and has the power to promote high standards
of training and public awareness on resuscitation.
In this study, respondents with CPR training
were more willing to perform it at home and in the
street (under emergency situations), presumably
as they had acquired enough knowledge and skills
to generate confidence and courage. The powerful
impact of CPR training on saving lives should
never be underestimated. Although only 15% of
the respondents without CPR training would like
to save others’ lives, nearly half of them (45%)
expressed willingness to perform CPR for their
family members if needed. The intimate relationship
among family members may be the motivation in
such cases. According to the AHA, 80% of sudden
cardiac arrests happen at home.7 Therefore, it makes
sense to exploit intimate emotions to facilitate and
publicise the CPR training, especially for those with
vulnerable members in their family.
In this study, the overall level of CPR
knowledge of the respondents was very low, with a
median of one correct answer out of eight questions,
which was in agreement with previous studies.11 20
Knowledge was particularly weak related to the
compression-to-ventilation ratio and appropriate
number of cardiac compressions per minute. This
could be because 79% of the respondents had not
received any CPR training, whereas 72% out of the
214 who had, recalled receiving it more than 2 years
earlier and 51% had received it more than 5 years
earlier. The AHA recommends its frequently revised
CPR guidelines based on rigorous scientific evidence
and the consensus opinions of experts. Using a
compression-to-ventilation ratio of 30:2 during
CPR for victims of all ages was a major update in
2005.30 In addition, the sequence of ‘A-B-C’ (Airway,
Breathing, Chest compression) was changed to
‘C-A-B’ (Chest compression, Airway, Breathing) in
the 2010 Guidelines.30 Therefore, knowledge about
up-to-date guidelines is likely to be most rewarding.
This survey did not explore why people
refused to perform CPR, which could be crucial
for raising bystander CPR rates in Hong Kong. As
indicated in one study from Japan, people had fear of
contracting transmitted diseases through mouth-to-mouth
ventilations.13 Legal liability could be another
concern. Therefore, public education and laws to
protect CPR providers appear necessary, for which
Good Samaritan laws need to be enacted. Certainly,
the reasons why Hong Kong citizens opt not to
undertake CPR warrant future surveys.
Conclusions
Knowledge of CPR in the Hong Kong public is still
poor. The percentage of citizens that have had CPR
training is relatively low. Unwillingness to perform
CPR is particularly common, especially among
those who have not received any CPR training. Government and non-government organisations
need to promote educational activities and explore
diverse approaches to reinforce and refresh the
content of training. Government needs to increase
public awareness of CPR and enact laws to protect
bystanders undertaking CPR. Incorporating CPR
training into the secondary school and college
curricula has also been suggested.
Declaration
The authors declare that there is no conflict of
interest.
Acknowledgement
The study was supported by the Nethersole School
of Nursing, Cardiovascular and Acute Care Research
Group Funding.
References
1. Travers AH, Rea TD, Bobrow BJ, et al. Part 4: CPR
Overview, 2010 American Heart Association Guidelines
for Cardiopulmonary Resuscitation and Emergency
Cardiovascular Care. Circulation 2010;122(18 Suppl 3):S676-84.
2. Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and
stroke statistics—2012 update: A report from the American
Heart Association. Circulation 2012;125:e2-e220. CrossRef
3. Nichol G, Thomas E, Callaway CW, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA 2008;300:1423-31. CrossRef
4. Chan PS, Jain R, Nallmothu BK, Berg RA, Susson C. Rapid response teams: a systematic review and meta-analysis. Arch Intern Med 2010;170:18-26. CrossRef
5. Lee K. The Hong Kong College of Cardiology automated external defibrillator programme. The Hong Kong Medical Diary 2008;13:14-6.
6. Sasson C, Rogers MA, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes 2010;3:63-81. CrossRef
7. Hazinski MF, Nolan JP, Billi JE, et al. Part 1: executive summary: 2010 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation 2010;122(16 Suppl 2):s250-75. CrossRef
8. Cave DM, Aufderheide TP, Beeson J, et al. Importance and implementation of training in cardiopulmonary resuscitation and automated external defibrillation in schools: a science advisory from the American Heart Association. Circulation 2011;123:691-706. CrossRef
9. Wong TW, Yeung KC. Out-of-hospital cardiac arrest: two and a half years experience of an accident and emergency department in Hong Kong. J Accid Emerg Med J 1995;12:34-9. CrossRef
10. Leung LP, Wong TW, Tong HK, Lo CB, Kan PG. Out-ofhospital cardiac arrest in Hong Kong. Prehosp Emerg Care 2001;5:308-11. CrossRef
11. Cheung BM, Ho C, Kou KO, et al. Knowledge of cardiopulmonary resuscitation among the public in Hong Kong: telephone questionnaire survey. Hong Kong Med J 2003;9:323-8.
12. Konstandions HD, Evangelos KI, Stamatis K, Thyresia S, Zacharenia AD. Community cardiopulmonary resuscitation training in Greece. Res Nurs Health 2008;31:165-71. CrossRef
13. Taniguchi T, Omi W, Inaba H. Attitudes toward the performance of bystander cardiopulmonary resuscitation in Japan. Resuscitation 2007;75:82-7. CrossRef
14. American Heart Association. 2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Part 3: overview of CPR. Circulation 2005;112:s12-8.
15. Hazinski MF, Gonzales L, O'Neill L, editors. BLS for healthcare providers: student manual. Dallas, TX: American Heart Association; 2006.
16. Hosmer DW, Lemeshow S. Applied logistic regression. 2nd ed. New York: John Wiley and Sons; 2000. CrossRef
17. Larsen P, Pearson J, Galletly D. Knowledge and attitudes towards cardiopulmonary resuscitation in community. N Z Med J 2004;117:U870.
18. Jennings S, Hara TO, Cavanagh B, Bennett K. A national survey of prevalence of cardiopulmonary resuscitation training and knowledge of the emergency number in Ireland. Resuscitation 2009;80:1039-42. CrossRef
19. Celenza T, Gennat HC, O'Brien D, Jacobs IG, Lynch DM, Jelinek GA. Community competence in cardiopulmonary resuscitation. Resuscitation 2002;55:157-65. CrossRef
20. Rasmus A, Czekajlo MS. A national survey of the Polish population's cardiopulmonary resuscitation knowledge. Eur J Emerg Med 2000;7:39-43. CrossRef
21. Sipsma K, Stubbs BA, Plorde M. Training rates and willingness to perform CPR in King Country, Washington: a community survey. Resuscitation 2011;82:564-7. CrossRef
22. Berden HJ, Willems FF, Hendrick JM, Pijls NH, Knape JT. How frequently should basic cardiopulmonary resuscitation training be repeated to maintain adequate skills? BMJ 1993;306:1576-7. CrossRef
23. Liu H, Clark AP. Cardiopulmonary resuscitation training for family members. Dimens Crit Care Nurs 2009;28:156-63. CrossRef
24. Blewer AL, Leary M, Decker CS, et al. Cardiopulmonary resuscitation training of family members before hospital discharge using video self-instruction: a feasibility trial. J Hosp Med 2011;6:428-32. CrossRef
25. Einspruch EL, Lynch B, Aufderheide TP, Nichol G, Becker L. Retention of CPR skills learned in a traditional AHA Heart-saver course versus 30-min video self-training: A controlled randomized study. Resuscitation 2007;74:476-86. CrossRef
26. Chung CH, Siu AY, Po LL, Lam CY, Wong PC. Comparing the effectiveness of video self-instruction versus traditional classroom instruction targeted at cardiopulmonary resuscitation skills for laypersons: a prospective randomised controlled trial. Hong Kong Med J 2010;16:165-70.
27. Uray T, Lunaer A, Ochsenhofer A, et al. Feasibility of lifesupporting first-aid (LSFA) training as a mandatory subject in primary schools. Resuscitation 2003;59:211-20. CrossRef
28. Hamasu S, Morimoto T, Kuramoto N, et al. Effects of BLS training on factors associated with attitude toward CPR in college students. Resuscitation 2009;80:359-64. CrossRef
29. Kanstad BK, Nilsen SA, Fredriken K. CPR knowledge and attitude to performing bystander CPR among secondary school students in Norway. Resuscitation 2011;82:1053-9. CrossRef
30. Field JM, Hazinski MF, Sayre MR, et al. Part 1: executive summary: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010;112(18 Suppl 3): S640-56. CrossRef