Hong Kong Med J 2014;20:45–51 | Number 1, February 2014 | Epub 11 Sep 2013
DOI: 10.12809/hkmj133899
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Elective unilateral total knee replacement using continuous femoral nerve blockade versus conventional patient-controlled analgesia: perioperative patient management based on a multidisciplinary pathway
Janet WS Wu, FHKCA, FHKAM (Anaesthesiology)1; YC Wong, FHKCOS2
1 Department of Anaesthesia, Yan Chai Hospital, Tsuen Wan, Hong Kong
2 Department of Orthopaedics and Traumatology, Yan Chai Hospital, Tsuen Wan, Hong Kong
Corresponding author: Dr JWS Wu (janetwuws@gmail.com)
Abstract
Objectives: To evaluate the effectiveness of our new multidisciplinary
pathway for total knee replacement patients and compare
outcomes after continuous femoral nerve blockade versus
conventional patient-controlled analgesia for postoperative
pain.
Design: Randomised controlled trial in a routine clinical setting.
Setting: Acute orthopaedic wards and operating theatres, Yan Chai
Hospital, Hong Kong.
Patients: Sixty patients underwent elective unilateral total knee
replacement under spinal anaesthesia from May 2009 to
September 2011 and were randomly assigned to continuous
femoral nerve blockade or conventional patient-controlled
analgesia (30 patients in each group).
Main outcome measures: Quality of pain control was evaluated by pain scores at rest and
during mobilisation, opioid consumption, frequency of side-effects,
and patient satisfaction score. Rehabilitation progress
was assessed according to the day of first starting weight-bearing
exercise, day of independent walking in the ward with aid,
Timed Up and Go test, and time elapsing till discharge. Surgical
outcome was assessed by the Knee Society score 6 months after
discharge, re-admissions, and occurrence of complications.
Results: Patients having continuous femoral nerve blockade tended to
have less pain on movement and achieved earlier mobilisation
than those having patient-controlled analgesia. The former
group consumed less opioids, had fewer side-effects, and were
more satisfied with their postoperative analgesia. Both groups
showed an equally high degree of satisfaction with the new
management pathway. Hospital stays, surgical outcomes, and
frequency of complications were similar in the two groups.
Conclusion: Continuous femoral nerve blockade proved to be a feasible
and better alternative mode of postoperative analgesia than
our conventional patient-controlled analgesia. Our new
multidisciplinary management pathway and multimodal analgesic
regimen featuring the continuous femoral nerve blockade
appeared beneficial to patients and effective in our clinical setting.
New knowledge added by this
study
- Levobupivacaine concentration as low as 0.08% provided adequate analgesia in our patients with minimal muscle weakness and mild numbness.
- Co-ordinated pathways featuring the use of continuous femoral nerve blockade were effective and appreciated by our patients.
- Work is necessary to identify areas of improvement to shorten hospital stays and hasten recovery without compromising outcomes and wellbeing.
- A multidisciplinary approach to total knee replacement patients can be applied to other surgical groups, for whom suitable studies should be conducted to investigate possible overall benefit.
Introduction
Total knee replacement (TKR) is commonly performed
to reduce chronic pain and improve the functional
state of patients suffering from degenerative disease.
A favourable patient outcome depends very much
on surgical technique, postoperative analgesia, and
active mobilisation. All these require input from
different specialties and carers,1 for which well-coordinated
clinical pathways on postoperative
management have been shown to reduce hospital
costs and improve quality of life of patients.2 3 4
Postoperative analgesia is an essential part of every
pathway.5 6 7 Choices for postoperative analgesia are
many. They include conventional patient-controlled
analgesia (PCA) and various neuraxial and peripheral
nerve blocks.8 9 In our new pathway, we featured the
use of continuous femoral nerve blockade (CFNB)
against our conventional PCA, because CFNB was
shown to provide better analgesia, reduce patient
opioid consumption and resulting side-effects.8 10
Various institutions also reported faster achievement
of discharge criteria,11 quicker mobilisation,12 and better recovery at 6-week postoperation.13 The use of
CFNB, together with a multimodal analgesic regimen,
can provide better postoperative pain relief and
hasten the speed of rehabilitation and mobilisation
while minimising the drug side-effects.14 15 16
Our new multidisciplinary pathway comprised
the following:
1. Introduction of CFNB against the conventional PCA, plus a standardised multimodal analgesic regimen (including a combination of paracetamol and sustained release diclofenate [Appendix 1] on optimising acute postoperative pain control).
2. Aggressive physiotherapy with early mobilisation, starting on postoperative day (POD) 1.
3. Active early screening for deep vein thrombosis (DVT) by ultrasonography on PODs 4-5.
4. Monitoring and treatment for complications, ensuring patient safety and satisfaction.
1. Introduction of CFNB against the conventional PCA, plus a standardised multimodal analgesic regimen (including a combination of paracetamol and sustained release diclofenate [Appendix 1] on optimising acute postoperative pain control).
2. Aggressive physiotherapy with early mobilisation, starting on postoperative day (POD) 1.
3. Active early screening for deep vein thrombosis (DVT) by ultrasonography on PODs 4-5.
4. Monitoring and treatment for complications, ensuring patient safety and satisfaction.
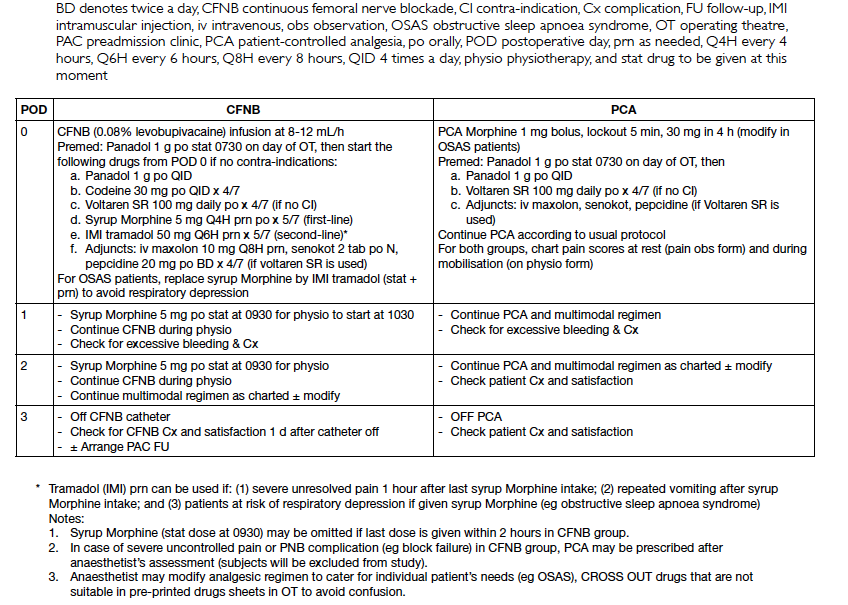
Appendix 1. Multimodal analgesic regimen for elective total knee replacement patients during study period
Methods
This was a randomised controlled trial using a
structured questionnaire and data retrieval forms, and
was conducted in orthopaedic wards and operating
theatres (OTs) in Yan Chai Hospital between May 2009
and September 2011. Prior approval from Kowloon
West Cluster Ethics Committee was obtained. The
target patients were those who underwent unilateral
elective TKR under spinal anaesthesia (SA). Patients
unable to communicate, had contra-indications to
peripheral nerve blockade, receiving anticoagulation
or DVT prophylaxis, and those eventually converted
to general anaesthesia or having complicated
revision surgery were excluded from the study. A
sample size of 60 patients was calculated based on
a Power Analysis and Sample Size calculator with a
background pain score of 0.6 (6/10), an expected
difference of 0.3 (3/10), an alpha of 0.05 (2-sided), and
power of 0.8. These 60 patients were randomised to
the CFNB and PCA groups (30 patients in each), using
computer-generated random numbers. Subjects
were divided into two groups (odd against even
numbers generated by the computer). The case
allocation was concealed in sealed envelopes and
the mode of analgesia revealed to case anaesthetist
and patient after the patient was included in the
study. No blinding was feasible for ward doctors,
nurses, and physiotherapists due to practical
constraints (different machine types being placed by
the bedside). All cases were managed according to
our new multidisciplinary TKR pathway (Appendix 2) and multimodal analgesic regimen (Appendix 1).
Data were extracted from the preoperative period till
6 months after discharge from hospital.
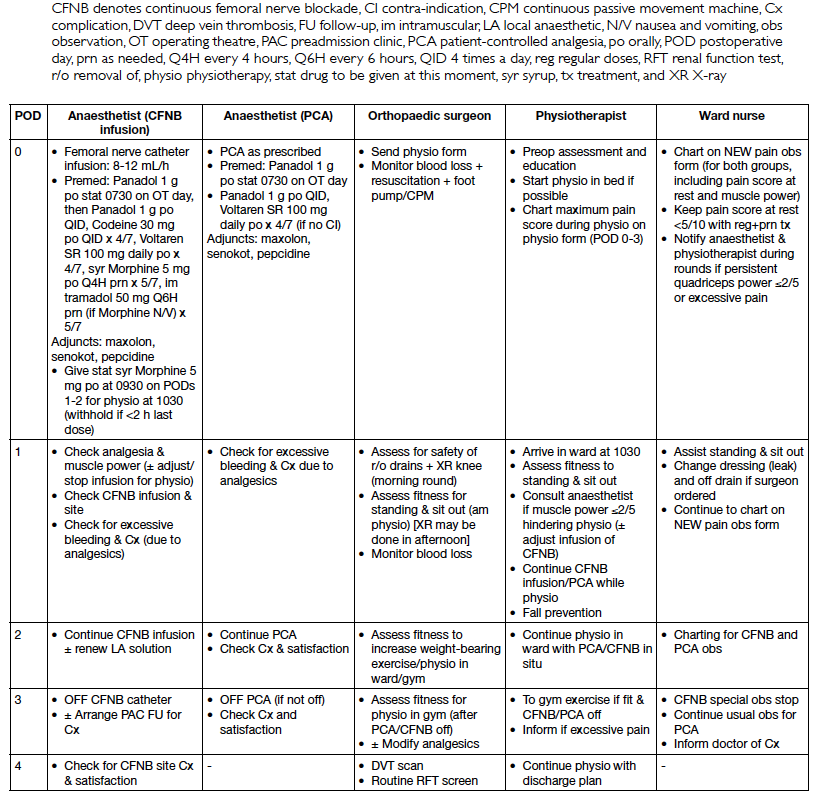
Appendix 2. Multimodal analgesic regimen + multidisciplinary protocol for patients undergoing total knee replacement during study period
For CFNB patients, the relevant catheter was
inserted under nerve stimulation and ultrasound
guidance, and before the performance of SA inside the OT a correct position was confirmed by the case
anaesthetist with ice and ultrasound in the induction/
recovery room. A standardised bolus of 15 mL 0.5%
levobupivacaine was injected after insertion of the
CFNB catheter. Successful femoral nerve blockade
was ensured by testing with ice before performance
of SA. Patients were then started on a continuous
infusion of 8 to 12 mL/h of 0.08% levobupivacaine
postoperatively in the recovery area till POD 3 (4-day
infusion regimen) when the catheter was removed
(in the ward by an anaesthetist). Regarding the PCA
patients, they were allowed intravenous morphine
after the operation, starting in the recovery area.
Both CFNB and PCA groups were started on
a standardised multimodal analgesic regimen (if
not contra-indicated) that entailed paracetamol,
sustained release diclofenate, opioids (codeine or
morphine), and drugs to prevent the side-effects
from these analgesics (Appendix 2).
Both patient groups received SA using a
25G Quincke spinal needle and local anaesthetics
injected intrathecally to achieve a block of at least
T10 for the surgery. Then they underwent TKR using
a tourniquet which was inflated to pressures of 250
to 280 mm Hg before skin incision. The tourniquet
was deflated after bandages were applied at the
end of surgery. Cement was used in all cases. A
drain was inserted using suction and reviewed by
surgeons and ward nurses on POD 1 (during the
surgeon’s morning round). At that round, decisions
were made as to whether the drain could be safely
removed, the patient was fit to go for X-ray, and
undergo mobilisation in the ward on that day (under
supervision of the physiotherapist). Thereafter, the
physiotherapist assessed the patient’s fitness to step
up the intensity of exercise in the ward and then in
the gymnasium of the Department of Physiotherapy
(without monitoring by a nurse). Until discharge,
each patient’s pain intensity and complications were
monitored closely by ward nurses and surgeons.
Routine ultrasound screening was performed
on PODs 4-5 to detect the early occurrence of DVT.
All patients had sequential leg compressors applied
and started on early mobilisation postoperatively
from POD 1 if possible (to prevent DVT).
Data were collected on the quality of pain
control (pain scores on visual analogue scale [VAS]
of 1-10 at rest and during mobilisation, supervised
by physiotherapist), opioid consumption and
the frequency of side-effects (by ward nurse and
anaesthetist doing pain rounds twice per day), patient
satisfaction score (VAS 1-10 on the quality of analgesia
by the pain anaesthetist), and discontinuation of PCA
or CFNB. The progress of rehabilitation (from the
day of mobilisation and independent walking in the
ward), the Timed Up and Go test (conducted by the
physiotherapist), and surgical outcomes were also recorded. Surgical outcomes entailed Knee Society
scores (assessed preoperatively, upon discharge,
and then 6 weeks and 6 months after discharge),
complications, re-admissions, and mortality (all
assessed by orthopaedic surgeons). All data were
analysed using the Statistical Package for the Social
Sciences (Windows version 10.0; SPSS Inc, Chicago
[IL], US), and outcome measures were compared
using Student’s t tests and Chi squared tests.
Results
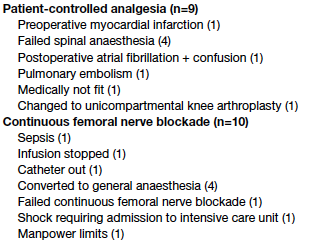
In all, 79 patients were recruited but 19 were excluded
for various reasons (Box), and replacements were
recruited using the permuted block technique.
Eventually 30 patients each were recruited as the
CFNB and PCA groups. Basic demographic data,
intra-operative surgical and anaesthetic parameters
in the two groups were similar (Table 1).
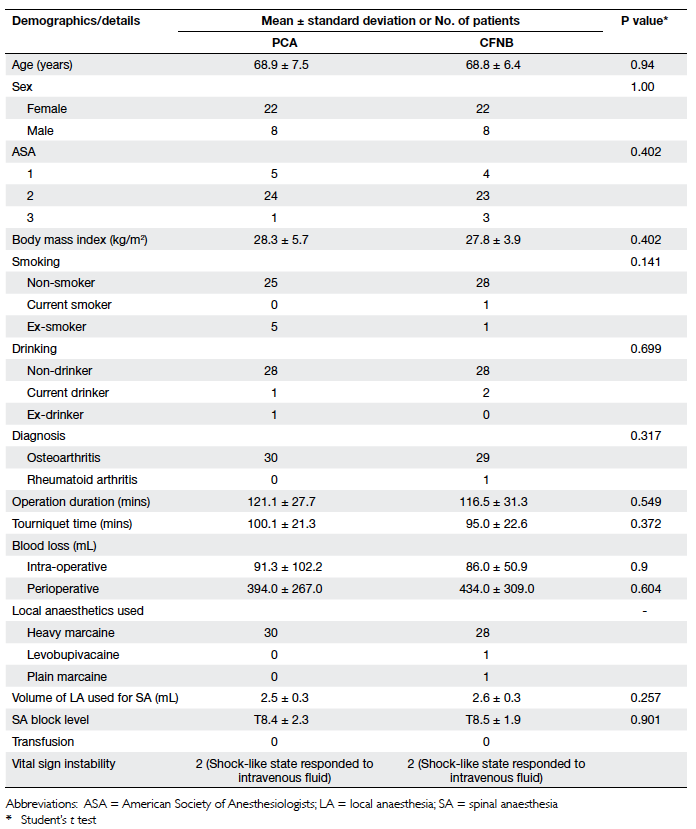
Table 1. Basic demographics, and surgical and anaesthetic details of the continuous femoral nerve blockade (CFNB) and conventional patient-controlled anaesthesia (PCA) groups
Regarding the quality of pain control, the
CFNB patients tended to have lower pain scores
during mobilisation on PODs 1 and 2 than those
in the PCA group (Table 2), but their pain scores at
rest were similar. For the sake of comparison, opioid
consumption of each patient was converted to
equivalent dosages of intravenous morphine. On this
basis, the CFNB group consumed significantly less
opioid than the PCA group only on PODs 0-1 (P<0.05),
but more opioid on POD 3 (Table 2). Fewer patients
suffered from opioid side-effects in the CFNB than
PCA group on all PODs (nausea and/or vomiting
27% vs 63%, and dizziness 17% vs 40%; P<0.05 for
both; Table 3). Mild catheter site oozing and mild
limb numbness were reported in about one third
of the CFNB patients. Notably, non-steroidal anti-inflammatory
drug (NSAID)–related complications
were rare in both groups. Patients were more satisfied
with the quality of pain control by CFNB than PCA
(Table 4; P=0.05). More patients would use the same
form of postoperative analgesia again for TKR in the
CFNB than PCA group (67% vs 50%, respectively).
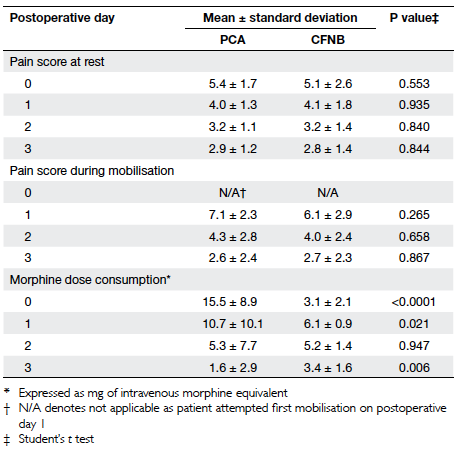
Table 2. Maximum pain scores at rest and during mobilisation, and opioid consumption of the continuous femoral nerve blockade (CFNB) and conventional patient-controlled anaesthesia (PCA) groups
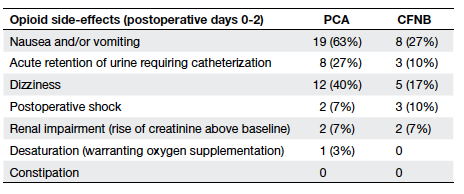
Table 3. Opioid side-effects in the continuous femoral nerve blockade (CFNB) and conventional patient-controlled anaesthesia (PCA) groups
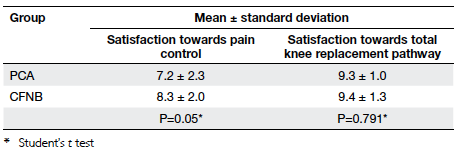
Table 4. Patients’ satisfaction score upon discharge from hospital of the continuous femoral nerve blockade (CFNB) and conventional patient-controlled anaesthesia (PCA) groups
Concerning rehabilitation, more CFNB than
PCA patients started mobilisation on POD 1 (83%
vs 50%, respectively, P=0.012; Table 5). The mean
day of independent walking in the ward was also
earlier (POD 6 vs 8; P=0.047). Significant dizziness,
and nausea and vomiting were the main reasons for
delayed early mobilisation in the PCA group. We were
unable to draw conclusions for the Timed Up and Go
test because of missing data (30%). No accidental fall, injury, or complaint was reported throughout the
study period.
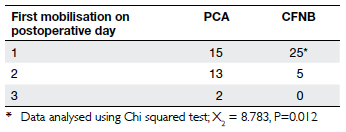
Table 5. Day of starting mobilisation of the continuous femoral nerve blockade (CFNB) and conventional patientcontrolled anaesthesia (PCA) groups
Regarding surgical outcomes, the mean
duration of hospitalisation, in-hospital surgical
complications (bleeding, DVT, sepsis, etc) and Knee
Society score and functional score changes from
the preoperative period till the 6-month follow-up
were similar in both groups (Table 6). In all, DVT was
detected in five patients (on PODs 4-5): three were in the PCA group (2 had a body mass index [BMI] of
>36 kg/m2). There was no other known predisposing
factor for DVT in either group, and no pulmonary
embolism or mortality was reported. Surgical
infection occurred in two patients (1 in each group),
for which they underwent re-operation.
As to the efficiency of our new TKR pathway,
introduction of CFNB analgesia caused only a
minimal effect on case turnover, as such cases were
sent to the OT earlier to allow prior performance of
the CFNB that was tested in the recovery/induction
area before the previous case ended. The mean
waiting time pending transferral to the OT after CFNB
insertion was 28 minutes, and the mean discharge
time from the OT to the recovery area was 6 minutes.
Performance of the nerve block entailed a mean
time of 32 minutes (all performed or supervised by
anaesthesia specialists). After the operation, however,
the CFNB group remained significantly longer in the
recovery area (62 vs 46 minutes, P=0.014). No major
mishap and/or patient complication (accidental fall,
chronic neuropathic pain, or mortality) was reported.
Both groups reported equally high satisfaction scores
for our new TKR pathway (>9/10, P=0.791; Table 4).
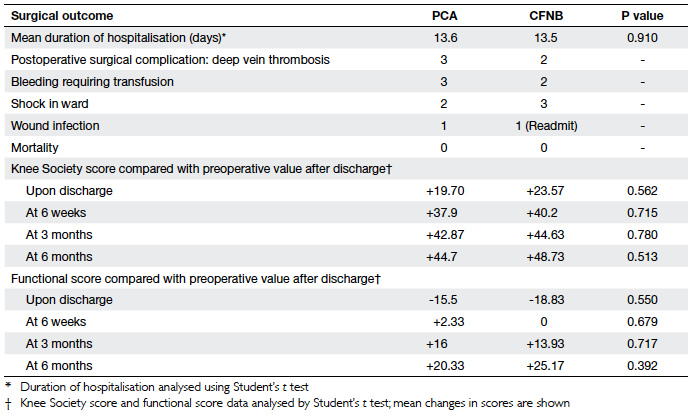
Table 6. Summary of surgical outcomes of the continuous femoral nerve blockade (CFNB) and conventional patient-controlled anaesthesia (PCA) groups
Discussion
For TKR patients, our results showed favourable
analgesic outcomes with the use of CFNB as
compared to conventional PCA. The former was
associated with lower pain scores during mobilisation
(not at rest) and reduced opioid consumption and
corresponding side-effects, which agreed well with
previous studies.8 12
A larger sample size or further addition of new analgesics to our current regimen may be necessary to reveal a statistically significant
difference in pain scores. Significantly more patients
were able to mobilise on POD 1 in the CFNB group,
which achieved better patient morale, and a sense
of control and satisfaction. Earlier mobilisation was
made possible due to better analgesia by CFNB and its
opioid-sparing effect caused fewer distressing side-effects
(nausea, vomiting, and dizziness). However,
there was possible unintended over-treatment with
opioids in the CFNB group from PODs 2-3 (when pain
intensity had dropped markedly). Modifications were
considered either to reduce the standard opioid
dosage or attempt earlier removal of the catheter
(on POD 2 instead of 3) so as to facilitate earlier
aggressive exercise in the physiotherapy gymnasium.
On the contrary, the PCA patients were less satisfied
with quality of pain control; most of their distress
being due to opioid-related side-effects that
hindered activation and interfered with mobilisation
on POD 1. There may have been under-utilisation of
opioids in both groups, because the patients choose
not to activate for further morphine boluses to avoid
nausea/vomiting and dizziness despite moderate pain; but the extent of this effect was not estimated. In
about two thirds of patients in both groups, NSAIDs
were prescribed and transient renal impairment on
POD 4 warranted stopping them in a few instances.
Routine monitoring of renal function on POD 3 was
not indicated, given our limited period of NSAID
prescription (4 days) and the low frequency of renal
impairment on POD 4.
Rehabilitation appeared to be faster with
CFNB. No accidental dislodgement of CFNB/PCA
catheters or patient injury was reported during
physiotherapy with the machines and catheters in
situ. The PCA group started independent walking
in the ward earlier than CFNB group was possibly
due to unavailability of services during weekends
and public holidays. This manpower limitation may
have affected less than 10% of our subjects, and was
overcome in the middle of the study, when surgeons
allocated more TKRs to be performed earlier in
the week to facilitate continued physiotherapy in
the immediate postoperative period. Long-term outcomes were similar as reflected by knee score
changes. Mobility and function were both improved.
Most patients were taking only simple analgesics (eg
paracetamol as required) for any residual pain.
In both groups, DVT occurred in a minority
of cases, with a frequency similar to that usually
encountered in our hospital (8-10%). All subjects were
encouraged to mobilise early to minimise DVT and
foot pumps were applied from POD 0; two patients
in PCA group were extremely obese (BMI >36 kg/m2).
In such patients, there may be co-existing obstructive
sleep apnoea and cardiovascular problems that
warrant intensive care unit monitoring. However, beds
may not always be available for such elective cases,
resulting in unwanted cancellations on the proposed
day of surgery. The role of CFNB, SA, and multimodal
analgesics appear essential in this situation, so as
to facilitate opioid sparing and reduce respiratory
depression in the general ward while providing
safer and better analgesia than PCA morphine. With
better co-ordination, CFNB can be safely used and
removed with concomitant use of low-molecular-weight
heparin in high-risk cases. After our study,
local guidelines have evolved to offer such patients
regional blocks together with anticoagulation.
The work logistics with the introduction of
CFNB to our TKR patients were efficient and different
carers co-ordinated well to minimise disturbance
to OT turnover and ensure patient safety and
comfort during the whole process of rehabilitation.
Despite achieving earlier mobilisation, we were unable to attain hospital stays shorter than 13 to 14 days (our pre-study standard), which was mostly
for social reasons including lack of home carers,
proper assistance for safe rehabilitation at home,
personnel to bring patients back for out-patient
follow-up and physiotherapy. Further collaboration
with occupational therapists and social workers and
preoperative psychosocial preparation for patients
and their families in the new pre-admission clinic are
essential, with a view to reducing hospital stays while
ensuring patient satisfaction and safety.
Sources of error
Selection bias may have occurred when 19 patients
were excluded from the original sample and may
not have had the same demographic profile as their
replacements (Table 1). When assessing for pain
and satisfaction scores, measurement bias may have
ensued when different ward nurses, anaesthetists,
and physiotherapists asked patients at different times
despite all of them having been instructed to ask
questions in the same way in Cantonese and using
the same VAS for comparison. Reported pain scores
may also be affected by other similar patients nearby,
and the carers not blinded to the mode of patient
analgesia. The effect of self-withholding of opioids
due to undesirable side-effect was not estimated (in both groups). Recall bias can occur when patients are
asked about their satisfaction with our TKR pathway,
as some may have left hospital already and the
anaesthetist could only call them for assessment after
discharge. Complete blinding of investigators and
assessors was not possible in our setting, as the PCA
and CFNB machines had very different appearances
and were mounted near the bedside to facilitate
easier and safer clinical care of analgesia.
Acknowledgements
Special thanks to the many dedicated colleagues
from the Department of Anaesthesia, Orthopaedics
and Traumatology, nursing teams of both orthopaedic
wards and operating theatres, Physiotherapy,
Occupational Therapy, social workers and pre-admission
clinic nurses and staff who put in much
effort to improve our service delivery and quality to
achieve better patient outcomes.
References
1. Ranawat CS, Ranawat AS, Mehta A. Total knee arthroplasty
rehabilitation protocol: what makes the difference? J
Arthroplasty 2003;18(3 Suppl 1):27S-30S. Crossref
2. Kim S, Losina E, Solomon DH, Wright J, Katz JN. Effectiveness
of clinical pathways for total knee and total hip arthroplasty:
literature review. J Arthroplasty 2003;18:69-74. Crossref
3. Yasunaga H, Tsuchiya K, Matsuyama Y, Ohe K. Analysis of
factors affecting operating time, postoperative complications,
and length of stay for total knee arthroplasty: nationwide
web-based survey. J Orthop Sci 2009;14:10-6. Crossref
4. Larsen K, Sørensen OG, Hansen TB, Thomsen PB, Søballe
K. Accelerated perioperative care and rehabilitation
intervention for hip and knee replacement is effective:
a randomized clinical trial involving 87 patients with 3
months of follow up. Acta Orthop 2008;79:149-59. Crossref
5. Department recommendation for pain control in total
knee replacement (TKR) surgery (1/7/2010). Hong Kong:
Department of Anaesthesia and Intensive Care, Tuen Mun
Hospital; 2010.
6. Clinical pathway—total knee replacement. Jan 2009.
Ontario, Canada: The Credit Valley Hospital; 2009.
7. Walter FL, Bass N, Bock G, Markel DC. Success of clinical
pathways for total joint arthroplasty in a community
hospital. Clin Orthop Relat Res 2007;457:133-7.
8. Paul JE, Arya A, Hurlburt L, et al. Femoral nerve block
improves analgesia outcome in total knee replacement.
Anesthesiology 2010;113:1144-62. Crossref
9. Chu CP, Yap JC, Chen PP, Hung HH. Postoperative outcome
in Chinese patients having primary total knee arthroplasty
under general anaesthesia/intravenous patient-controlled
analgesia compared to spinal-epidural anaesthesia/analgesia. Hong Kong Med J 2006;12:442-7.
10. Chelly JE, Greger J, Gebhard R, et al. Continuous femoral
blocks improve recovery and outcome of patients undergoing
total knee arthroplasty. J Arthroplasty 2001;16:436-45. Crossref
11. Ilfeld BM, Le LT, Meyer RS, et al. Ambulatory continuous
femoral nerve blocks decrease time to discharge readiness
after tricompartment total knee arthroplasty: a randomized,
triple-masked, placebo-controlled study. Anesthesiology
2008;108:703-13. Crossref
12. Ilfeld BM, Mariano ER, Girard PJ, et al. A multicenter,
randomized, triple-masked, placebo-controlled trial of the
effect of ambulatory continuous femoral nerve blocks on
discharge readiness following total knee arthroplasty in
patients on general orthopedic wards. Pain 2010;150:477-84. Crossref
13. Carli F, Clemente A, Asenjo JF, et al. Analgesia and functional
outcome after total knee arthroplasty: periarticular
infiltration vs continuous femoral nerve block. Br J Anaesth
2010;105:185-95. Crossref
14. Hebl JR, Dilger JA, Byer DE, et al. A pre-emptive multimodal
pathway featuring peripheral nerve block improves
perioperative outcomes after major orthopedic surgery. Reg
Anesth Pain Med 2008;33:510-7. Crossref
15. Parvataneni HK, Shah VP, Howard H, Cole N, Ranawat
AS, Ranawat CS. Controlling pain after total hip and
knee arthroplasty using a multimodal protocol with local
periarticular injections: a prospective randomized study. J
Arthoplasty 2007;22(6 Suppl 2):33S-38S. Crossref
16. Fischer HB, Simanski CJ, Sharp C, et al. A procedure-specific
systematic review and consensus recommendations
for postoperative analgesia following total knee arthroplasty.
Anaesthesia 2008;63:1105-23. Crossref