Hong Kong Med J 2025;31:Epub 2 Dec 2025
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Absence of the left coronary artery complicated
with acute myocardial infarction: a case report
Yu Liu#, MD, PhD, Guoyuan Zhao#, MM, Xianliang Wang, MD, PhD, Jingyuan Mao, MD, PhD, Zhiqiang Zhao, MD, PhD
First Teaching Hospital of Tianjin University of Traditional Chinese Medicine/National Clinical Research Center for Chinese Medicine
Acupuncture and Moxibustion, Tianjin, China
# Equal contribution
Corresponding author: Dr Zhiqiang Zhao (quanmingzhao@126.com)
Case presentation
A 67-year-old Asian female with no family history
of heart disease was admitted to the Department
of Psychosomatic Diseases at our hospital on 30
November 2024, primarily for intermittent anxiety
and a 2-week history of general malaise but also
headache, stomachache, backache, a sensation
of choking and throat pain, dyspnoea, and,
occasionally, a feeling of impending death. After
attending a psychiatric hospital she was diagnosed
with anxiety and prescribed oral flupentixol
and melitracen tablets, zaleplon and oxazepam.
Upon admission to the department, symptomatic
interventions including anxiolytics and sleep aids
were administered. On 3 December 2024 at 9:01 am,
the patient abruptly encountered back pain. During
the episode, the patient appeared to be choking
but reported no perspiration or chest pain. Urgent
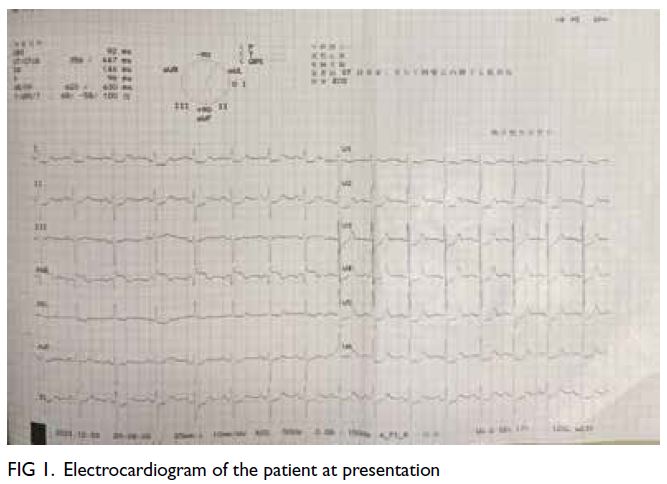
electrocardiogram revealed ST segment elevation of
0.2 to 0.25 mV in the augmented vector right lead
and depression of 0.2 to 0.35 mV in lead I, augmented
vector left lead, lead II, and leads V1 to V5 (Fig 1). The high-sensitivity troponin was 0.061 ng/mL (normal,
<0.016 ng/mL). In view of the suspected acute
myocardial infarction, the patient was transferred
to the Coronary Care Unit. Emergency coronary
angiography revealed 90% stenosis in the proximal
segment of the right coronary artery (RCA). The left
anterior descending artery (LAD) and left circumflex
artery were obscured in various angiographic views,
while the blood flow in the distal segment of the
RCA could be observed. Intravascular ultrasound
examination of the RCA revealed a minimum lumen
area of 2.59 mm2 at the lesion site, with a plaque
burden of 91%. Subsequent to balloon dilation, a
single everolimus-eluting stent (PROMUS Element
Plus; Boston Scientific, Marlborough [MA], United
States) was implanted. Postoperatively there was
no residual stenosis at the RCA lesion site, and
distal blood flow was classified as TIMI III (the
Thrombolysis in Myocardial Ischemia Trial III) [Fig 2a-d]. Postoperatively, the patient reported no pain
in the precordial region or back.
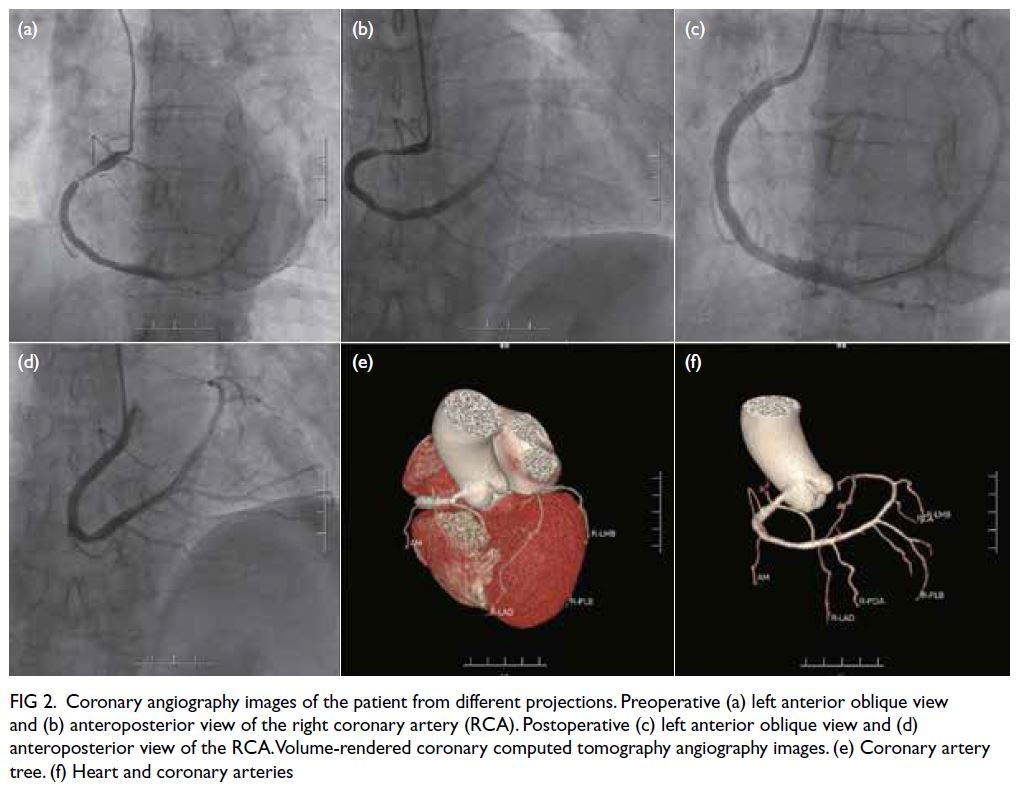
Figure 2. Coronary angiography images of the patient from different projections. Preoperative (a) left anterior oblique view and (b) anteroposterior view of the right coronary artery (RCA). Postoperative (c) left anterior oblique view and (d) anteroposterior view of the RCA. Volume-rendered coronary computed tomography angiography images. (e) Coronary artery tree. (f) Heart and coronary arteries
Coronary computed tomography angiography
(CTA) [Fig 2e and f] revealed that the left main trunk,
LAD, and left circumflex artery did not arise from
the left coronary sinus. The RCA originated from the
right coronary sinus. These results aligned with the
findings of coronary angiography. Echocardiography
revealed that the left ventricular ejection fraction
was 60% with mild mitral regurgitation and reduced
left ventricular diastolic function. The patient’s
condition improved after treatment and she was
discharged home on 10 December. At 1-month
follow-up, the patient reported no chest tightness,
shortness of breath, or precordial pain, and ECG
showed no signs of ischaemia.
Discussion
A single coronary artery (SCA) is an uncommon
coronary artery anomaly (CAA). The congenital
absence of the left coronary artery (LCA) is an
uncommon subtype of SCA, occurring with an
incidence rate of 0.024%, with no discernible gender
disparity.1 In 1979, Lipton classified SCA into types
I, II, and III based on coronary origin, branching pattern, and disease course.2 In our patient, the
single RCA was type R-I. As myocardial ischaemia
is the aetiology of cardiovascular events induced
by CAAs, coronary angiography is vital. Prior to
percutaneous coronary intervention, a meticulous
assessment of the surgical treatment strategy is
essential.
The SCA form of CAA typically presents with no
clinical symptoms and lacks specificity. Our patient
exhibited cardiac-related symptoms, including
backache, a sensation of choking, throat pain, and
dyspnoea. Nonetheless the simultaneous occurrence
of symptoms such as headache, stomachache and
general malaise prompted a diagnosis of anxiety
disorder. Coronary angiography was conducted to
assess the extent of vascular stenosis but revealed
the absence of an LCA, complicated by 90% stenosis
in the proximal segment of the RCA. The lesion
in the proximal segment of the patient’s RCA
was comparable to that in the left main trunk.
Thereafter, under intravascular ultrasound guidance,
the coronary artery lesions were assessed, and a
therapeutic approach was planned. Coronary CTA
is crucial for identifying aberrant openings and
congenital anomalies and unequivocally confirmed the congenital absence of the LAD in our patient.
Secondary prevention of coronary heart disease
is essential for these patients, ensuring proper
maintenance of the lumen in the distal vessels of the
RCA that supply the anterior and lateral walls.
Conclusion
The congenital absence of the LCA is an uncommon
condition with an often non-specific clinical
presentation. Clinically, if patients exhibit symptoms
of angina pectoris or electrocardiogram alterations
indicative of ischaemia, coronary CTA or coronary
angiography should be promptly conducted to
exclude congenital cardiovascular malformations.
This enables clinicians to accurately diagnose and
implement appropriate management.
Author contributions
All authors contributed to the concept or design of the study,
acquisition of data, analysis or interpretation of data, drafting
of the manuscript, and critical revision of the manuscript for
important intellectual content. All authors had full access to
the data, contributed to the study, approved the final version
for publication, and take responsibility for its accuracy and
integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
The study was funded by:
(1) Study of the Mechanism of Yangyin Shuxin Formula Inhibiting Calcium Overload in Cardiomyocytes through PI3K/IP3R Pathway, Improving Ejection Fraction, and Preserving Diastolic Function in Heart Failure, Key Research Project of Traditional Chinese Medicine in Tianjin (Ref No.: A0101); and
(2) Study on the immune-inflammatory mechanism of optimizing the polarization of macrophages mediated by IL-17 in Xinshengmaisan targeting myocardial fibrosis, Research Fund of the First Affiliated Hospital of Tianjin University of Traditional Chinese Medicine (Ref No.: XB2024006).
The funders had no role in the study design, data collection/ analysis/interpretation, or manuscript preparation.
(1) Study of the Mechanism of Yangyin Shuxin Formula Inhibiting Calcium Overload in Cardiomyocytes through PI3K/IP3R Pathway, Improving Ejection Fraction, and Preserving Diastolic Function in Heart Failure, Key Research Project of Traditional Chinese Medicine in Tianjin (Ref No.: A0101); and
(2) Study on the immune-inflammatory mechanism of optimizing the polarization of macrophages mediated by IL-17 in Xinshengmaisan targeting myocardial fibrosis, Research Fund of the First Affiliated Hospital of Tianjin University of Traditional Chinese Medicine (Ref No.: XB2024006).
The funders had no role in the study design, data collection/ analysis/interpretation, or manuscript preparation.
Ethics approval
The study was approved by the Institutional Review Board
of The First Teaching Hospital of Tianjin University of
Traditional Chinese Medicine, China (Ref No.: TYLL2024[Z]).
Written informed consent was obtained from the patient for
all treatments and procedures, and for the publication of this
case report (including the accompanying clinical images).
References
1. Sampath A, Chandrasekaran K, Venugopal S, et al. Single
coronary artery left (SCA L)–right coronary artery arising
from mid-left anterior descending coronary artery: new
variant of Lipton classification (SCA L-II) diagnosed by
computed tomographic angiography. Echocardiography
2020;37:1642-5. Crossref
2. Lipton MJ, Barry WH, Obrez I, Silverman JF, Wexler L.
Isolated single coronary artery: diagnosis, angiographic
classification, and clinical significance. Radiology
1979;130:39-47. Crossref