Hong Kong Med J 2025;31:Epub 10 Nov 2025
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
LETTER TO THE EDITOR
Vitamin B12 deficiency needs to be adequately
diagnosed and treated
TK Kong, FRCP, FHKAM (Medicine)
Division of Geriatric Medicine, Department of Medicine, The University of Hong Kong, Hong Kong SAR, China
Corresponding author: Dr TK Kong (tkkong@hku.hk)
To the Editor—A 79-year-old Chinese male presented
in January 2023 with a 2-week history of depressed
mood and a 2-year history of forgetfulness. He had
no recollection of his COVID-19 illness in December
2022, after which his memory further worsened.
He had been experiencing intermittent dyspepsia
since May 2012, with a finding of Helicobacter
pylori–negative inactive mild chronic antral gastritis
in September 2015, for which he took antacids,
famotidine, and pantoprazole as required. Review
of his history revealed a diagnosis of vitamin B12
deficiency anaemia 10 years earlier in September
2013 when he presented with depression, tiredness,
dizziness, weight loss, hand numbness, and laboratory
findings of macrocytic anaemia (haemoglobin level:
8.2 g/dL, mean cell volume [MCV]: 130.9 fL) along
with a low serum vitamin B12 level (<37 pmol/L).
He was treated with intramuscular cyanocobalamin
for 1 year followed by oral cyanocobalamin 100 mcg
twice a day for 2.5 years. His symptoms improved
and haemoglobin level, MCV (13.7 g/dL and 93.2fL,
respectively, June 2014; 15.1g/dL and 93.7 fL,
respectively, December 2016) and serum vitamin
B12 level (513 pmol/L, September 2014) normalised.
Examination in January 2023 revealed mildly impaired
cognition, depressed mood and positive Romberg
test, but no pallor or glossitis. A clinical diagnosis of
relapsed pernicious anaemia with neuropsychiatric
presentation was made and confirmed by a low
serum vitamin B12 level (<109 pmol/L, January 2023)
and a positive intrinsic factor antibody, although his
haemoglobin level and MCV were normal (14.0 g/dL
and 97.3 fL, respectively). His mood improved but
cognition remained unchanged after high-dose
oral vitamin B12 (mecobalamin 500 mcg 3 times a
day), with normalisation of serum vitamin B12 level
(318 pmol/L, April 2023). The patient was treated
in accordance with the Declaration of Helsinki.
Informed consent was obtained for publication of
this case.
This case illustrates the importance of
determining the aetiology of vitamin B12 deficiency,
failure to do so may lead to under-treatment and
disease relapse or progression. Pernicious anaemia
requires lifelong treatment with either parenteral or
high-dose (≥1 g daily) oral vitamin B12. Clinicians and
pathologists should be familiar with both classic and
non-classic presentations, causes, and laboratory
diagnosis of vitamin B12 deficiency, a common
treatable disorder (Table).1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 Neuropsychiatric
presentations can occur in the absence of anaemia or macrocytosis and may be non-classic (eg, depression, long COVID-19, hallucinations).1 2 3 4 5 6
Underlying causes, often multiple in an individual,
need to be diagnosed, and persistent cause(s) require
lifelong treatment.1 Although acid-suppressive
drugs may have contributed to this patient’s vitamin
B12 deficiency (food-cobalamin malabsorption),7
intrinsic factor antibody positivity and dyspepsia
history point to an additional cause in autoimmune
atrophic gastritis. The classic histopathology of this
condition should be confirmed by gastric biopsy,
including both corpus and antrum.8 Periodic
screening for metformin-induced vitamin B12
deficiency in diabetes, though proposed over 50
years ago,9 has only recently been incorporated into
guidelines,1 10 but is not widely practised.
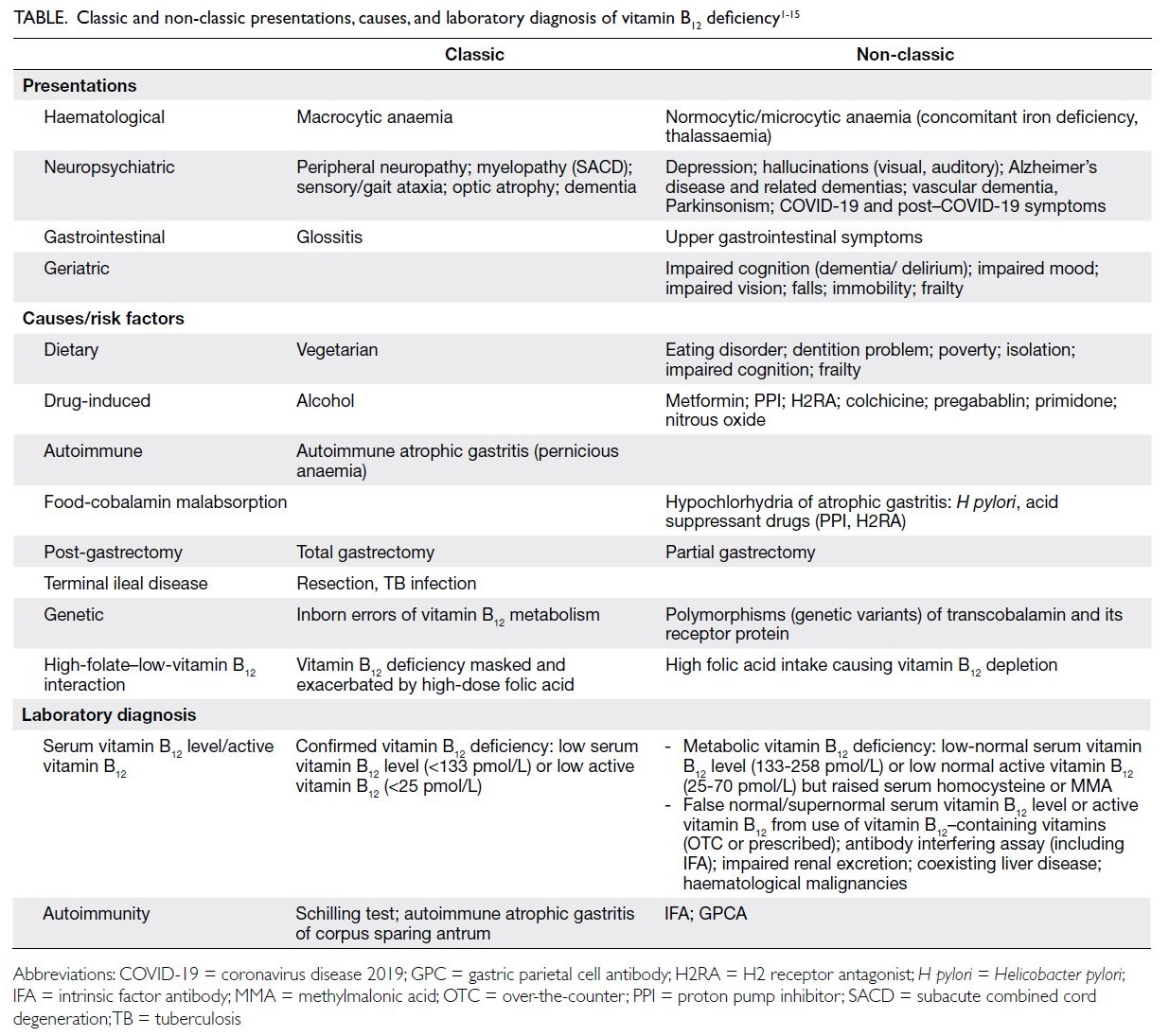
Table. Classic and non-classic presentations, causes, and laboratory diagnosis of vitamin B12 deficiency1 2 3 4 5 6 7 8 9 10 11 12 13 14 15
Vitamin B12 deficiency can occur in individuals
with apparently normal or supernormal serum
vitamin B12 or active vitamin B12 levels, and clinicians
should be aware of factors that affect test results
(Table).1 2 4 11 12 The 2024 National Institute for
Health and Care Excellence guideline1 introduced an
indeterminate range for low-normal serum vitamin
B12 or active vitamin B12 levels that necessitates further
tests for raised serum homocysteine or methylmalonic
acid (Table) to confirm the diagnosis in those with
risk factors and compatible manifestations of vitamin
B12 deficiency. Because of the limitations of vitamin
B12 levels, the diagnosis and monitoring of treatment
adequacy should not depend solely on its level, but
should instead be guided by clinical judgement and
response.1 Although a low vitamin B12 level in patients
on replacement therapy suggests poor adherence or
inadequate dosing, a normal or high level does not
necessarily indicate adequate treatment and should
not prompt reduction discontinuation.1 The clinical
response should be assessed at follow-up instead
of merely repeating vitamin B12 levels.1 Individual
variability in vitamin B12 treatment response and
dose requirement has been observed, possibly due to
genetic variants of transcobalamin and its receptor.
These variants may reduce vitamin B12 availability and
reduce energy metabolism, ultimately contributing
to frailty.1 2 13
Author contributions
The author solely contributed to the concept or design of the
paper, acquisition of the data, analysis or interpretation of the
data, drafting of the manuscript, and critical revision of the
manuscript for important intellectual content. The author had
full access to the data, contributed to the paper, approved the final version for publication, and takes responsibility for its
accuracy and integrity.
Conflicts of interest
The author has disclosed no conflicts of interest.
Funding/support
This letter received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
1. National Institute for Health and Care Excellence. Vitamin
B12 deficiency in over 16s: diagnosis and management.
NICE guideline; 2024. Available from: https://www.nice.org.uk/guidance/ng239. Accessed 10 Aug 2025.
2. McCaddon A. Vitamin B12 in neurology and ageing; clinical
and genetic aspects. Biochimie 2013;95:1066-76. Crossref
3. Lindenbaum J, Healton EB, Savage DG, et al.
Neuropsychiatric disorders caused by cobalamin deficiency
in the absence of anemia or macrocytosis. N Engl J Med
1988;318:1720-8. Crossref
4. Rietsema WJ. Unexpected recovery of moderate cognitive
impairment on treatment with oral methylcobalamin. J Am
Geriatr Soc 2014;62:1611-2. Crossref
5. Batista KS, Cintra VM, Lucena PA, et al. The role of vitamin
B12 in viral infections: a comprehensive review of its relationship with the muscle-gut-brain axis and implications
for SARS-CoV-2 infection. Nutr Rev 2022;80:561-78. Crossref
6. Blom JD. Hallucinations and vitamin B12 deficiency: a
systematic review. Psychopathology 2024;57:492-503. Crossref
7. Andrès E, Affenberger S, Vinzio S, et al. Food-cobalamin
malabsorption in elderly patients: clinical manifestations
and treatment. Am J Med 2005;118:1154-9. Crossref
8. Neumann WL, Coss E, Rugge M, Genta RM. Autoimmune
atrophic gastritis—pathogenesis, pathology and
management. Nat Rev Gastroenterol Hepatol 2013;10:529-41. Crossref
9. Tomkin GH, Hadden DR, Weaver JA, Montgomery DA.
Vitamin-B12 status of patients on long-term metformin
therapy. Br Med J 1971;2:685-7. Crossref
10. Medicines and Healthcare products Regulatory Agency.
Metformin and reduced vitamin B12 levels: new advice for
monitoring patients at risk. Drug Safety Update. 11 Jun
2022. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1084085/June-2022-DSU-PDF.pdf . Accessed 10 Aug 2025.
11. Yang DT, Cook RJ. Spurious elevations of vitamin B12 with
pernicious anemia. N Engl J Med 2012;366:1742-3. Crossref
12. Delgado JA, Pastor García MI, Jiménez NM, et al.
Challenges in the diagnosis of hypervitaminemia B12.
Interference by immunocomplexes. Clin Chim Acta
2023;541:117267. Crossref
13. Matteini AM, Walston JD, Bandeen-Roche K, et al.
Transcobalamin-II variants, decreased vitamin B12
availability and increased risk of frailty. J Nutr Health
Aging 2010;14:73-7. Crossref
14. Mahmud K, Ripley D, Swaim WR, Doscherholmen A.
Hematologic complications of partial gastrectomy. Ann
Surg 1973;177:432-5. Crossref
15. Selhub J, Miller JW, Troen AM, Mason JB, Jacques PF.
Perspective: the high-folate–low-vitamin B-12 interaction
is a novel cause of vitamin B-12 depletion with a specific
etiology—a hypothesis. Adv Nutr 2022;13:16-33. Crossref

