Hong Kong Med J 2015 Oct;21(5):394–400 | Epub 14 Aug 2015
DOI: 10.12809/hkmj144310
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Clinical value of transforaminal epidural steroid injection in lumbar radiculopathy
SM Leung, MMed(Pain Mgt)(Syd), FHKAM (Orthopaedic Surgery)1,2;
WW Chau, MSc (Epi & Biostat)3;
SW Law, MOM, FHKAM (Orthopaedic Surgery)1,2,4;
KY Fung, MB, BS, FHKAM (Orthopaedic Surgery)1,2,4
1 Department of Orthopaedics and Traumatology, Alice Ho Miu Ling Nethersole Hospital, Tai Po, Hong Kong
2 Department of Orthopaedic Rehabilitation, Tai Po Hospital, Tai Po, Hong Kong
3 Department of Orthopaedics and Traumatology, The Chinese University of Hong Kong, Shatin, Hong Kong
4 Department of Orthopaedics and Traumatology, Prince of Wales Hospital, Shatin, Hong Kong
Corresponding author: Dr SM Leung (lsm457@ha.org.hk)
Abstract
Objectives: To identify the diagnostic, therapeutic,
and prognostic values of transforaminal epidural
steroid injection as interventional rehabilitation for
lumbar radiculopathy.
Design: Case series.
Setting: Regional hospital, Hong Kong.
Patients: A total of 232 Chinese patients with
lumbar radiculopathy attributed to disc herniation
or spinal stenosis received transforaminal epidural
steroid injection between 1 January 2007 and 31
December 2011.
Interventions: Transforaminal epidural steroid injection.
Main outcome measures: Patients’ immediate
response, response duration, proportion of patients
requiring surgery, and risk factors affecting the responses
to transforaminal epidural steroid injection for
lumbar radiculopathy.
Results: Of the 232 patients, 218 (94.0%) had a
single level of radiculopathy and 14 (6.0%) had
multiple levels. L5 was the most commonly affected
level. The immediate response rate to transforaminal
epidural steroid injection was 80.2% in 186 patients
with clinically diagnosed lumbar radiculopathy and
magnetic resonance imaging of the lumbar spine
suggesting nerve root compression. Of patients
with single-level radiculopathy and multiple-level
radiculopathy, 175 (80.3%) and 11 (78.6%) expressed
an immediate response to transforaminal epidural
steroid injection, respectively. The analgesic effect
lasted for 1 to <3 weeks in 35 (15.1%) patients, for
3 to 12 weeks in 37 (15.9%) patients, and for more
than 12 weeks in 92 (39.7%) patients. Of the 232
patients, 106 (45.7%) were offered surgery, with 65
(61.3%) undergoing operation, and with 42 (64.6%)
requiring spinal fusion in addition to decompression
surgery. Symptom chronicity was associated with
poor immediate response to transforaminal epidural steroid
injection, but not with duration of pain reduction. Poor response to transforaminal
epidural steroid injection was not associated with a
preceding industrial injury.
Conclusions: The immediate response to
transforaminal epidural steroid injection was
approximately 80%. Transforaminal epidural steroid
injection is a useful diagnostic, prognostic, and short-term
therapeutic tool for lumbar radiculopathy.
Although transforaminal epidural steroid injection
cannot alter the need for surgery in the long term, it
is a reasonably safe procedure to provide short-term
pain relief and as a preoperative assessment tool.
New knowledge added by this
study
- This is the first local study to evaluate the clinical value of transforaminal epidural steroid injection (TFESI) as an alternative to or antecedent procedure for definitive spinal surgery.
- TFESI is a reasonably safe diagnostic and therapeutic option as interventional rehabilitation for lumbar radiculopathy.
Introduction
Lumbar radiculopathy can be well-managed
conservatively in the primary health care setting,
but many patients with persistent disabling radicular
pain need attention in a specialty clinic. The majority
of patients first attend a public specialty clinic in
Hong Kong with pain chronicity of more than 12
months, as they have had no significant clinical
response to conservative management in primary
health care, private medical specialists, traditional
Chinese medicine, or alternative medicine, and they
anticipate a long waiting time in a public hospital.
Epidural steroid injection is commonly practised by
orthopaedic surgeons, neurosurgeons, rehabilitation
specialists, pain specialists, and interventional
radiologists worldwide. The thresholds for offering
epidural steroid injection by clinicians and
acceptance by patients are variable, however.
Transforaminal epidural steroid injection
(TFESI) is one of the more common approaches
of epidural steroid injection, along with the
interlaminar and caudal approaches. The technique
is target-specific and the best route for delivering
medication to the ventral epidural space (Fig 1a) and dorsal root ganglion,1 where most pathological
changes occur.2 3 The least amount of drug with a
relatively higher drug concentration is required to
reach the primary site of pathology compared with
interlaminar and caudal epidural steroid injections.4
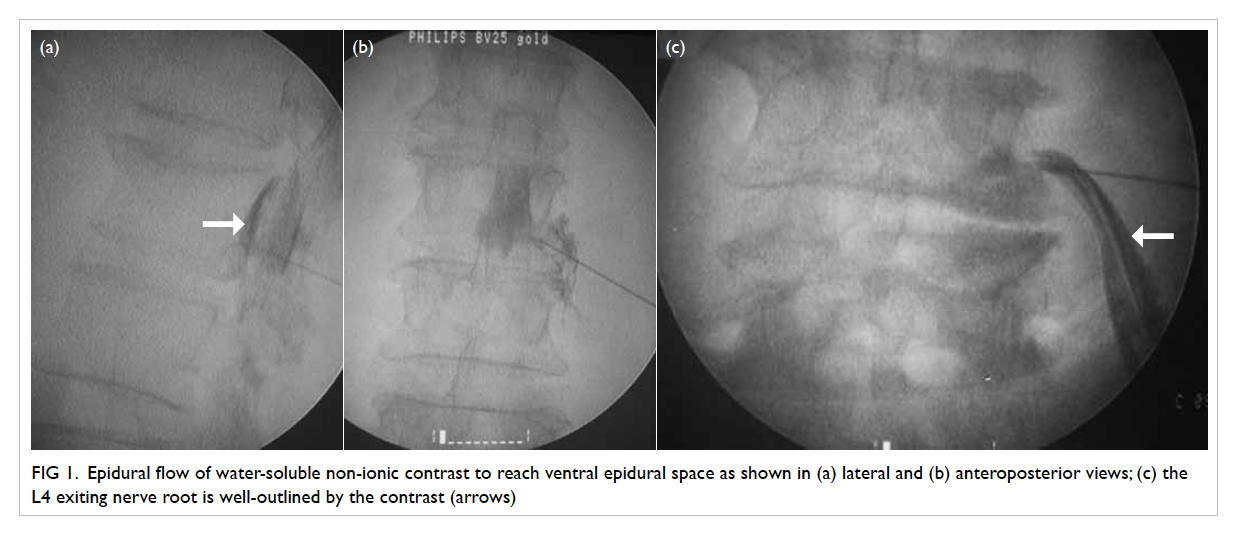
Figure 1. Epidural flow of water-soluble non-ionic contrast to reach ventral epidural space as shown in (a) lateral and (b) anteroposterior views; (c) the L4 exiting nerve root is well-outlined by the contrast (arrows)
Transforaminal epidural steroid injection is
a useful procedure for lumbar radiculopathy.5 The
technique provides neural blockade to anaesthetise
the target nerve root for diagnostic purposes, and
interrupts nociceptive input and self-sustaining
activity of the neurons. Steroid provides anti-inflammatory
effect (inhibition of pro-inflammatory
synthesis and release of mediators) and produces
longer-term pain relief, primarily for radiculopathy.
The prognostic value of TFESI for surgical outcomes
has been reported, with better surgical outcome in
TFESI responders with chronic lumbar radiculopathy
than in non-responders.6 The technique, however,
does not alter the ultimate need for surgery.7
Underlying sepsis, malignant disease, and
coagulopathy are considered to be contra-indications
for spinal injection. The perceived benefits and
threshold of offering TFESI as an adjunct to
conservative treatment for patients with lumbar
radiculopathy attributed to disc herniation or spinal
stenosis are variable among orthopaedic surgeons,
rehabilitation specialists, and pain specialists. The
objective of this study was to identify the diagnostic,
therapeutic, and prognostic values of TFESI for
lumbar radiculopathy in Chinese patients in Hong
Kong.
Methods
Procedural steps for transforaminal epidural steroid injection
Patients were placed in the prone position on a
radiolucent operating table. A 22-G spinal needle
was inserted into the target neuroforamen with
fluoroscopic image guidance. The target nerve
root and its epidural space were outlined by water-soluble
non-ionic contrast, ensuring epidural flow
of contrast with no intravascular, intradural, or
subcutaneous infiltration (Fig 1). A mixture of
1-mL methylprednisolone acetate 40 mg and 1-mL
bupivacaine 0.5% was injected. Finally, the intact
spinal needle was removed.
Data collection and analysis
All patients who received TFESI for lumbar
radiculopathy at Alice Ho Miu Ling Nethersole
Hospital, Hong Kong from 1 January 2007 to 31
December 2011 (5 years) were identified by the
electronic medical record system in the hospital.
Retrospective review of all the medical records
identified patients with numeric pain rating scale
score (NPRS) of 4 to 7 (out of 10) who took less than
three types of analgesics for at least 8 weeks as
conservative treatment, or patients with persistent
disabling pain with NPRS of >7 despite taking more
than three types of analgesics for at least 1 week as
conservative treatment. Patients with NPRS of <4,
missing record of post-procedure response, or who
had received previous lumbar spinal injection and
lumbar spinal surgery were excluded.
The first part of the study assessed the response
rate to diagnostic block by the local anaesthetic effect
of TFESI for all patients with a clinical diagnosis of
lumbar radiculopathy attributed to disc herniation or
spinal stenosis, with compatible magnetic resonance
imaging (MRI) findings of laterality and affected
level. The second part of the study assessed the
therapeutic and prognostic values of the steroid effect
of TFESI as an adjunct to conservative treatment
prior to assessment of surgical need.
The threshold for surgery for patients with
lumbar radiculopathy attributed to prolapsed
intervertebral disc (PID) and spinal stenosis,
in general, considered factors of disabling pain
resulting in inability to meet activity demands,
clinical MRI findings compatible for laterality and
site of compression, and medical fitness for general
anaesthesia and major spinal surgery. Spinal fusion
might be considered for patients with concomitant
spondylolisthesis with instability or anticipated
instability resulting from optimal surgical
decompression in the lateral recess or foraminal
stenosis and concomitant disabling discogenic low
back pain that has not responded to conservative
treatment.
An immediate response on the procedure day
was considered to have a positive diagnostic value.
Patients who reported pain reduction of greater than
50% at the first follow-up visit 4 weeks after TFESI
were considered to have a positive therapeutic
response to the steroid effects. The response
duration, proportion of patients finally requiring
surgery, whether decompression alone or spinal
fusion besides decompression was needed, and risk
factors that affected the response to TFESI were
retrospectively reviewed.
Comparisons were carried out for all patients,
as well as patients with PID or spinal stenosis only.
Associations between responses to TFESI and risk
factors for symptom chronicity and industrial injury
were done by Fisher’s exact test or Mann-Whitney U
test where appropriate. Non-parametric tests were
done because some continuous variables were not
normally distributed. The Statistical Package for the
Social Sciences Windows version 20.0 (SPSS Inc,
Chicago [IL], US) was used for all statistical analysis.
A two-sided P value of ≤0.05 was considered
statistically significant.
Results
A total of 241 patients were recruited into this study.
Nine patients were excluded for the following reasons:
TFESI responders with PID and L5 radiculopathy
had had symptom duration of less than 1 week and
TFESI was not considered to be adequate first-line
conservative treatment (n=3); and TFESI immediate
responders did not return for first follow-up (n=2)
and TFESI responses were not documented in the
medical records (n=4) so the response durations for
these six patients could not be verified. Therefore,
the total number of eligible participants was 232
(110 men and 122 women; mean age ± standard
deviation [SD]: 55.6 ± 14.3 years). The mean age
of patients with PID and spinal stenosis were 37.4
± 7.5 years and 60.3 ± 11.7 years, respectively. The
symptom chronicity ranged from 8 days to 23 years
with a median of 12.0 months, as well as 25th, 75th, and
90th percentiles being 7.0, 36.0,
and 60.0 months, respectively in patients with lumbar
radiculopathy. No statistically significant difference
(P=0.402) in symptom chronicity between the PID
and spinal stenosis groups was noted (median
[interquartile range] duration: PID group 12.0 [8.0-24.0] months vs spinal stenosis group 12.0 [6.0-36.0]
months). Fewer PID patients (n=48; 20.7%) needed
TFESI than spinal stenosis patients (n=184; 79.3%)
with lumbar radiculopathy in the study period.
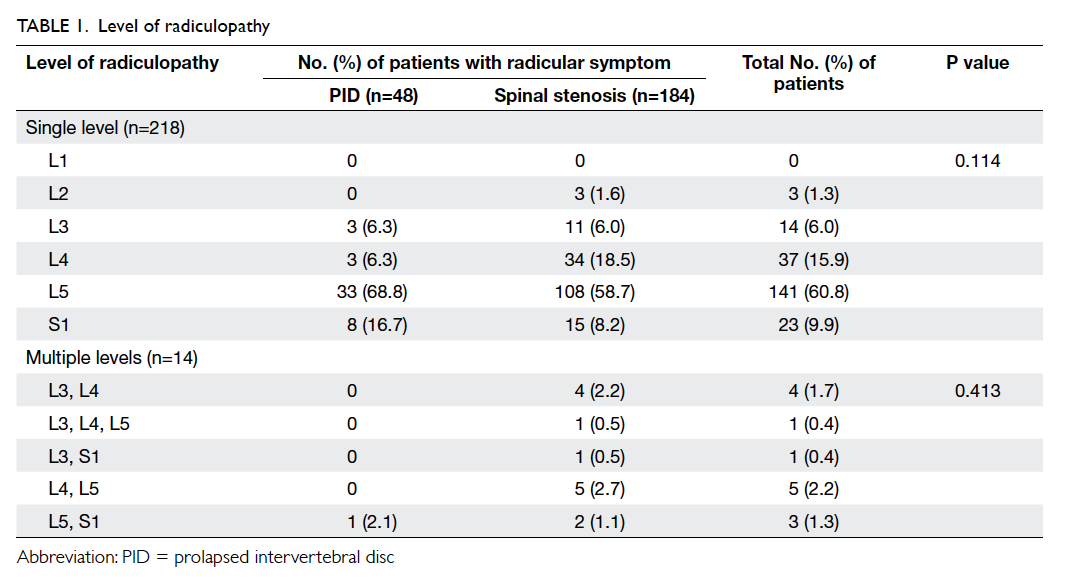
L5 was the most commonly affected level of
radiculopathy (n=150; 64.7%) regardless of whether
a patient had single or multiple levels or underlying
pathology of PID or spinal stenosis (Table 1). Therefore, post-ganglionic block of the L5 nerve root
by L5-S1 TFESI was most commonly done.
Diagnostic value of transforaminal epidural steroid injection
The immediate response rate to TFESI was 80.2% in 186 patients with clinically diagnosed lumbar
radiculopathy and MRI of the lumbar spine
suggesting nerve root compression. Overall, 218
(94.0%) patients were affected at a single level and
14 (6.0%) were affected at multiple levels (Table 1).
The immediate response rates to TFESI were 175
(80.3%) in the single-level radiculopathy group and
11 (78.6%) in the multiple-level radiculopathy group.
There was no statistically significant difference in
the immediate responder rate between patients with
PID or spinal stenosis (P=0.877). No complications
were reported.
Predictive value for final need for surgery
The final need for surgery of TFESI immediate
responders was noted in 10/39 (25.6%) patients in the PID
group and 43/147 (29.3%) patients in the spinal
stenosis group (Table 2).
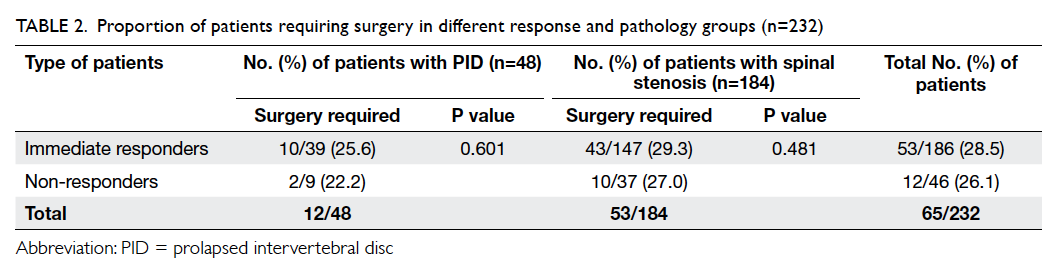
Table 2. Proportion of patients requiring surgery in different response and pathology groups (n=232)
Of the 232 patients, 106 (45.7%) were offered
surgery, of whom 65 (61.3%) accepted surgery. The
mean time from TFESI to uptake of surgery was 7.9
months. There was a statistically significant shorter
median time to definitive surgery in the PID group
(10.0 months) than in the spinal stenosis group (19.2
months) [P<0.01]. This reflects the fact that PID
patients with failed first-line conservative treatment
who needed TFESI for lumbar radiculopathy were
likely to accept surgery earlier than patients with
spinal stenosis. Patients with PID were younger
(mean age, 37.0 years) than spinal stenosis patients
(mean age, 59.2 years) undergoing surgery, which
might be related to less daily activity demand, higher
perceived operative risks, and older people being
more psychologically reluctant to undergo surgery.
Of the 65 surgical patients, 23 (35.4%)
underwent decompression surgery alone, with a
mean time from TFESI of 5.45 months (SD, 5.25 months;
median, 3.6 months; range, 8 days to 17.63 months).
The remaining 42 (64.6%) patients required spinal
fusion in addition to decompression surgery, with
a mean time from TFESI of 9.37 months (SD, 7.23
months; median, 7.22 months; range, 14 days to
25.33 months). The difference in time to surgery
for these two groups was statistically significant
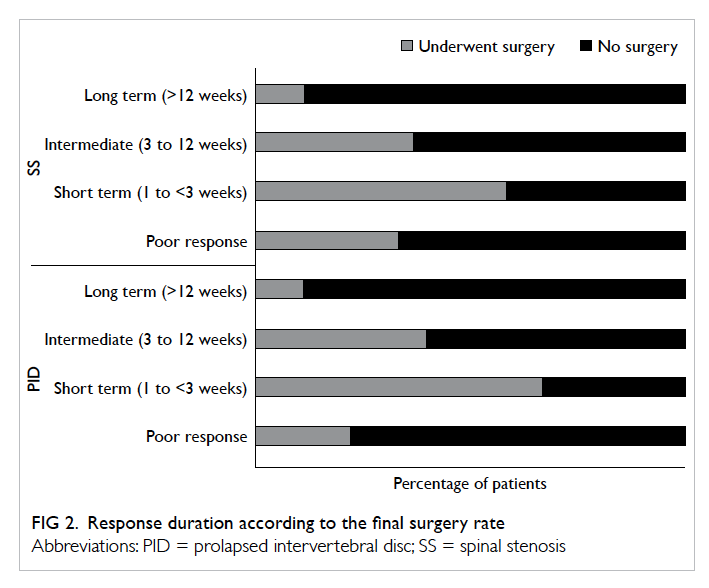
(P=0.012). More patients with a short-term response
to TFESI underwent surgery (Fig 2) and TFESI was commonly used as a preoperative assessment tool.
Association between response to transforaminal epidural steroid injection and duration of pain relief
The analgesic effect of TFESI lasted for less than 1
week (poor response) in 68 (29.3%) patients, for 1
to <3 weeks (short term) in 35 (15.1%) patients, for
3 to 12 weeks (intermediate) in 37 (15.9%) patients,
and for more than 12 weeks (long term) in 92
(39.7%) patients. More patients with spinal stenosis
underwent surgery in the short-term pain reduction
group (1-<3 weeks), and the association between
response to TFESI and surgery for spinal stenosis
was significant (P<0.01), but no significance was
noted for PID patients (P=0.067) [Table 3].
Association between poor response to transforaminal epidural steroid injection and chronicity of symptoms and industrial injury
Poor response (mean, 34.3 ± 50.9 months) to TFESI (no immediate response and
pain reduction duration of <1 week) was significantly
associated with chronicity of symptoms (vs 23.1 ± 28.3 months in patients with positive response) [P=0.047]. Pain
reduction duration had no significant association
with symptom chronicity for pain reduction of less
than 3 months and 3 months or more in the PID
(P=0.225) and spinal stenosis (P=0.250) groups
(Table 4).
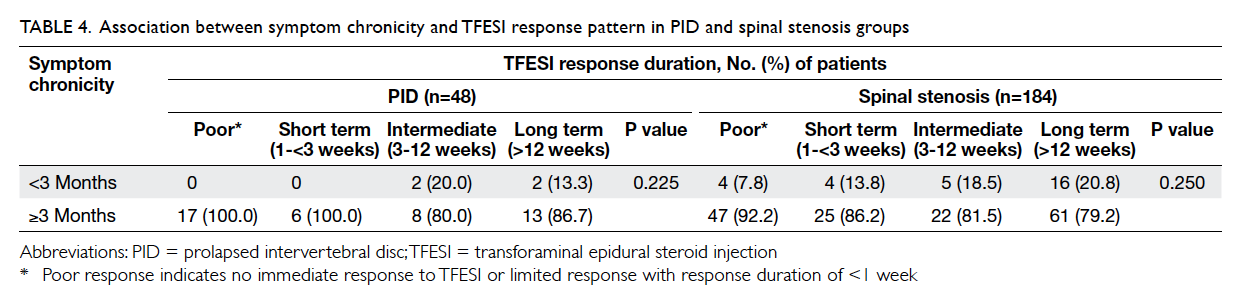
Table 4. Association between symptom chronicity and TFESI response pattern in PID and spinal stenosis groups
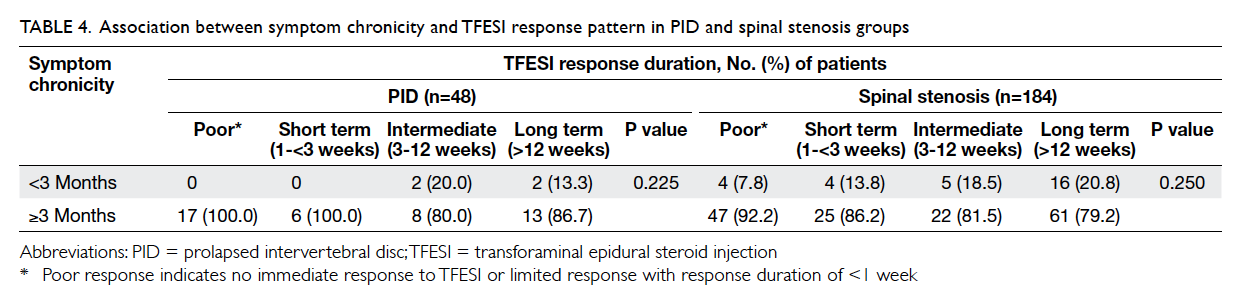
Table 4. Association between symptom chronicity and TFESI response pattern in PID and spinal stenosis groups
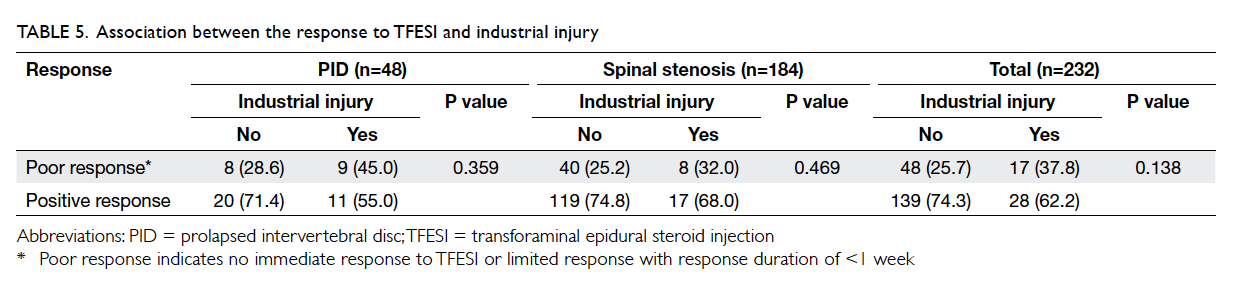
There was no association between response to
TFESI and industrial injury for all eligible patients
(P=0.138) and no significant association according
to the underlying cause of PID (P=0.359) and spinal
stenosis (P=0.469) [Table 5].
Discussion
The decision by clinicians to offer a treatment and
by patients to accept it is often determined by the
perceived benefits, likelihood of success, and the
cost (eg risks, time cost, labour cost, and financial
cost) of the treatment. In real-world clinical practice,
there are large variations in the perceived benefits
and likelihood of success of TFESI among clinicians
despite its relatively fewer risks and lower cost
than spinal surgery. This retrospective case review
attempted to show real-life practice in a local unit
during a fixed period to evaluate the diagnostic,
prognostic, and therapeutic values.
Lumbar radiculopathy can be well managed conservatively, but many patients still have persistent
disabling radicular pain needing attention in a
specialty clinic. Most patients first attended a public
specialty clinic with chronicity of more than 12
months because of no significant clinical response to
conservative management. Most patients receiving
spinal injection have had a lengthy period of trying
various modalities of conservative treatments,
reflected by a median time of 12 months of symptom
chronicity for patients receiving TFESI.
The threshold of offering TFESI as a diagnostic
tool and/or a therapeutic adjunct to conservative
treatment is variable among clinicians, reflected by
the wide variation of symptom chronicity from 8 days
to 23 years among the 232 patients receiving TFESI
in this study. Other factors affecting the threshold
of offering TFESI include severe neuropathic pain
not controlled by more than three kinds of high-dose
analgesic combinations that act on different
pain pathways, and the diagnostic need for doubtful
clinical MRI correlations, especially among patients
contemplating surgery or who are undergoing a pain
relief procedure while waiting for definitive surgery
in a local public hospital.
L5 radiculopathy was the most commonly
affected level, regardless of whether single or
multiple levels were affected, in patients with PID or
spinal stenosis in this series. Post-ganglionic block
of the L5 nerve root by L5-S1 TFESI was commonly
performed.
The clinical presentation of lumbar
radiculopathy without significant neurocompression
on MRI scan might be related to chemical irritation
by local inflammation from an annular tear rather
than significant mechanical compression to the nerve
root. These patients can be treated conservatively or
by TFESI. Sometimes, dynamic spinal stenosis as a
result of an incompetent degenerative disc with loss
of disc height and its support of the spinal load or
spondylolisthesis with spinal instability might be
worsened in the upright posture, and might not
be well demonstrated in MRI of the lumbar spine
taken in the supine position. The technique of TFESI
is a target-specific diagnostic tool to the affected
nerve root. The procedure increases the diagnostic
confidence of clinical lumbar radiculopathy before
both the patient and surgeon commit to more
invasive surgical interventions, especially for a
clinical diagnosis of lumbar radiculopathy with
doubtful correlation to MRI findings.
As demonstrated in this study, TFESI is a
target-specific diagnostic tool with up to 80%
immediate response for lumbar radiculopathy. An
immediate pain response is expected to be related
to the local anaesthetic effect acting on the affected
nerve root and its dorsal root ganglion, washout
effects of injectates on the chemical irritation of the
local inflammatory mediators or, occasionally, on
the loose extraforaminal sequestrated disc material.
The pain reduction duration is expected to be related
to the anti-inflammatory effect of steroid. However,
it is not expected to change the anatomy, which is
due to significant mechanical compression to the
affected nerve root. This often needs to be managed
surgically so the results of TFESI cannot alter the
final need for surgery.
Patients commonly enquire whether TFESI is
an alternative or antecedent procedure to definitive
spinal surgery. There is strong evidence to support
the use of lumbar TFESI in patients with acute-to-subacute unilateral radicular pain caused by
herniated nucleus pulposus or spinal stenosis.8 9
Nonetheless, there is no relief of pain in patients
with chronic failed back surgery syndrome and
documented fibrosis of the nerves.2
Chronic pain and industrial injury generally
have less favourable responses to many treatments.
This study showed significant differences in
symptom chronicity and poor immediate response
rate to TFESI (P=0.047), but failed to show a
statistically significant association between symptom
chronicity and TFESI response duration in lumbar
radiculopathy attributed to PID (P=0.225) or spinal
stenosis (P=0.250) [Table 4]. The diagnostic value of TFESI is more prominent than the therapeutic
value in chronic lumbar radiculopathy in both
the PID and spinal stenosis groups. A preceding
history of industrial injury was not associated with
TFESI response difference in lumbar radiculopathy
attributed to PID (P=0.359) or spinal stenosis
(P=0.469) [Table 5]. Therefore, industrial injury is not a limitation in consideration of offering TFESI.
As demonstrated in this study, most patients
(80.2%) with lumbar radiculopathy attributed
to PID or spinal stenosis were managed by non-surgical
treatments. Less than one-half of patients
(45.7%, 106/232) were offered surgery and only
65 (61.3%) of 106 patients accepted surgery. The
technique of TFESI is a reasonable therapeutic
trial as an alternative procedure, especially in older
frail patients with multiple medical co-morbidities
and high peri-operative risks. There were no
complications related to the injected medication or
needle placement in this series. The technique is a
reasonable, safe procedure provided that there is
radiographic verification of epidural flow of water-soluble
non-ionic contrast with no intravascular,
intradural, or subcutaneous infiltration.10
Nonetheless, there was still a sizable proportion
of patients (45.6%) who underwent surgery for
persistent disabling pain when there was clinical MRI–compatible neurocompression. The mean time to
surgery from TFESI was 7.9 months. The technique of
TFESI helps give time for better quality of pain relief,
but it does not affect the ultimate need of surgery,
especially for patients who require spinal fusion for
spinal instability, either anticipated preoperatively or
after surgical decompression. Among the 186 immediate responders,
up to 10 (25.6%) of 39 in the PID group and 43 (29.3%)
of 147 in the spinal stenosis group required surgery
(Table 2). Although TFESI is unable to correct structural pathology, it is a reasonable antecedent
procedure to definitive surgical decompression. The
technique provides 80.2% immediate response, thus
increasing the diagnostic confidence and providing
short-term pain reduction enabling patients to
remain active with reduced analgesic consumption
and associated systemic side-effects while awaiting
definitive spinal surgery. In addition, TFESI provides
a better quality of pain relief to help maintain
functional independence and to reduce hospital stay.
The procedure has a reasonably good diagnostic
utility and cost-effectiveness in patients considered
for lumbar decompression surgery.11
A limitation of this retrospective case review
is that the results were based on subjective self-reported
pain response, because a more objective
functional assessment was not always available in the
patients’ medical records. A prospective controlled
trial is warranted in the future to obtain more
comprehensive information about the change in
patients’ daily function in relation to pain reduction.
Conclusions
L5 radiculopathy is the most commonly affected
level of lumbar radiculopathy. The local anaesthetic
effect of TFESI is a useful diagnostic adjunct, with
up to 80.2% immediate response in patients with
lumbar radiculopathy. Although TFESI cannot
alter the need for spinal surgery, it is a reasonably
safe procedure to provide short-term pain relief to
allow patients to stay active with reduced analgesic
consumption and associated systemic side-effects
while awaiting surgery.
Declaration
The authors do not have any conflicts of interest to declare.
References
1. Bhargava A, DePalma MJ, Ludwig S, Gelb D, Slipman CW.
Injection therapy for lumbar radiculopathy. Curr Opin
Orthop 2005;16:152-7. Crossref
2. Rho ME, Tang CT. The efficacy of lumbar epidural steroid
injections: transforaminal, interlaminar, and caudal
approaches. Phys Med Rehabil Clin N Am 2011;22:139-48. Crossref
3. Roberts ST, Willick SE, Rho ME, Rittenberg JD. Efficacy of
lumbosacral transforaminal epidural steroid injections: a
systematic review. PM R 2009;1:657-68. Crossref
4. Abdi S, Datta S, Trescot AM, et al. Epidural steroids in the
management of chronic spinal pain: a systematic review.
Pain Physician 2007;10:185-212.
5. Botwin KP, Gruber RD, Bouchlas CG, et al. Fluoroscopically
guided lumbar transformational epidural steroid injections
in degenerative lumbar stenosis: an outcome study. Am J
Phys Med Rehabil 2002;81:898-905. Crossref
6. Derby R, Kine G, Saal JA, et al. Response to steroid
and duration of radicular pain as predictors of surgical
outcome. Spine (Phila Pa 1976) 1992;17(6 Suppl):S176-83. Crossref
7. Wilson-MacDonald J, Burt G, Griffin D, Glynn C. Epidural
steroid injection for nerve root compression. A randomised,
controlled trial. J Bone Joint Surg Br 2005;87:352-5. Crossref
8. Karppinen J, Malmivaara A, Kurunlahti M, et al.
Periradicular infiltration for sciatica: a randomized
controlled trial. Spine (Phila Pa 1976) 2001;26:1059-67. Crossref
9. Ng L, Chaudhary N, Sell P. The efficacy of corticosteroids
in periradicular infiltration for chronic radicular pain:
a randomized, double blind, controlled trial. Spine
2005;30:857-62. Crossref
10. Ptaszynski A, Huntoon M. Complications of spinal
injections. Tech Reg Anesth Pain Manag 2007;11:122-32. Crossref
11. Beynon R, Hawkins J, Laing R, Higgins N, Whiting P.
The diagnostic utility and cost-effectiveness of selective
nerve root blocks in patients considered for lumbar
decompression surgery: a systematic review and economic
model. Health Technol Assess 2013;17:88. Crossref