Hong Kong Med J 2017 Aug;23(4):333–9 | Epub 10 Mar 2017
DOI: 10.12809/hkmj164949
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Medium-term results of ceramic-on-polyethylene
Zweymüller-Plus total hip arthroplasty
H Li, MD1*;
S Zhang, MD2*;
XM Wang, MD3;
JH Lin, MD1;
BL Kou, MD1
1 Arthritis Clinic and Research Center, Peking University People’s Hospital, Beijing, No.11 Xizhimen South Street, Xicheng District, Beijing, 100044, China
2 Orthopaedic Department, Beijing Dongchengqu First People’s Hospital,
Beijing, 100075, China
3 Orthopaedic Department, Beijing Moslem Hospital, Beijing, 100054, China
* The first two authors contributed equally to this work.
Corresponding authors: Dr JH Lin (jianhao_lin@hotmail.com), Dr BL Kou (bolongkoublk@163.com)
Abstract
Introduction: The need for better durability and
longevity in total hip arthroplasty for patients with
various hip joint diseases remains a challenge.
This study aimed to obtain medium-term
results at a follow-up of >10 years
for Zweymüller-Plus total hip arthroplasty with
ceramic-on-polyethylene bearing.
Methods: A retrospective study was conducted to
review the results after a minimum of 12.4 years
of 207 consecutive total hip arthroplasties in 185
patients in Peking University People’s Hospital
in China using the Zweymüller SL-Plus stem in
combination with the Bicon-Plus threaded cup and
ceramic-on-polyethylene bearing between October
1994 and April 2000.
Results: During the study period, two patients
(2 hips) died and 25 patients (28 hips) were lost
to follow-up. Two hips were revised for aseptic
loosening of the Bicon-Plus cup. The mean clinical
and radiological follow-up was 14.1 years (range,
12.4-16.5 years) for the remaining 156 patients
(175 hips). The mean (standard deviation) Harris Hip score for the 175 hips increased significantly from
39.3 (3.8) preoperatively to 94.1 (2.5) postoperatively
at a mean follow-up of 14.1 years (P<0.05). Focal
osteolysis was observed in seven (4.0%) of 175 stems
and three (1.7%) of 175 cups. The Kaplan-Meier survival
with revision for any reason as the end-point was
99.03% (95% confidence interval, 95%-100%).
Conclusions: The high survival rate of the cementless
Zweymüller-Plus system with ceramic-on-polyethylene
bearing at mid-term follow-up makes
this total hip arthroplasty system reliable for patients
with various hip joint diseases.
New knowledge added by this study
- This study determined the medium-term outcome of Zweymüller-Plus total hip arthroplasty (THA) with ceramic-on-polyethylene bearing.
- Zweymüller-Plus THA has a good medium-term outcome and is reliable for patients with various hip joint diseases.
Introduction
Total hip arthroplasty (THA) is considered one
of the most effective therapies for a variety of
hip joint diseases. The cemented THA has been
successfully performed since the 1960s but has been
widely criticised in several postoperative follow-up
studies for its later loosening.1 2 During the 1970s,
cementless THA with different principles of fixation
and various new materials was introduced. This
prosthesis had good biocompatibility and its specific
surface structure could achieve secondary fixation to
bone that could avoid later loosening.3
The Zweymüller-Plus system (Smith &
Nephew Orthopaedics AG; Rotkreuz, Switzerland), a
kind of cementless THA that comprises the SL-Plus
stem and Bicon-Plus cup, was introduced in 1993 as
a successor to the Alloclassic system.4 It has been
widely used for primary THA. Because of aseptic
loosening due to polyethylene wear, alternative
bearings were introduced.5 6 These alternative
bearings included metal-on-metal, ceramic-on-ceramic,
and ceramic-on-polyethylene articulation.7 8
The Zweymüller-Plus THA system with the ceramic-on-polyethylene bearing has been reported to have
superior survival and durability at 10 years’ follow-up
than other bearings.9 Additionally, in the mid-1990s in mainland China, the
Zweymüller-Plus THA
with ceramic-on-polyethylene bearing was the most
common type of hip prosthesis. We report the results
after a minimum of 12.4 years of an independent
series using Zweymüller-Plus THA with ceramic-on-polyethylene bearing in a historical follow-up
study.
Methods
Between October 1994 and April 2000, a total
of 207 Zweymüller-Plus total hip replacements
(Smith & Nephew Orthopaedics AG) with ceramic-on-polyethylene bearings were performed in 185
consecutive patients at Peking University People’s
Hospital in China. The institutional review board of
Peking University People’s Hospital approved this
study, with the requirement of patient informed
consent waived because of its retrospective nature.
Patients
Data on the patients including gender, age, hip
distribution, initial diagnosis, complications, reason
for revisions, and clinical outcome were obtained
from the hospital database and retrospectively
reviewed. Basic demographic data and indications
for implantation of the prosthesis were collected.
Implants
The acetabular component was the Bicon-Plus cup
(Smith & Nephew Orthopaedics AG), a biconical threaded cup made of hot-forged
pure titanium (Fig 1). The Bicon-Plus cup has a microroughness of 4-6 µm and no coating on the
microporous outer surface. The polyethylene inlay
of the Bicon-Plus cup is made of conventional ultra-high-molecular-weight polyethylene that has been
sterilised by gamma irradiation.
The femoral component was the SL-Plus stem,
a cementless, rectangular, dual-tapered straight
stem made of a wrought Ti-6Al-7Nb alloy with a
microporous surface roughness of 4-6 µm (Smith &
Nephew Orthopaedics AG; Rotkreuz, Switzerland;
Fig 1). The femoral head with a diameter of 28 mm was made of high-grade alumina ceramics (the
third-generation alumina ceramics). The edges
of the SL-Plus stem were rounded to reduce the
occurrence of distal femoral cortical thickening. The
combination of polyethylene inlay with the 28-mm
diameter ceramic femoral head constituted the
ceramic-on-polyethylene bearing surface.
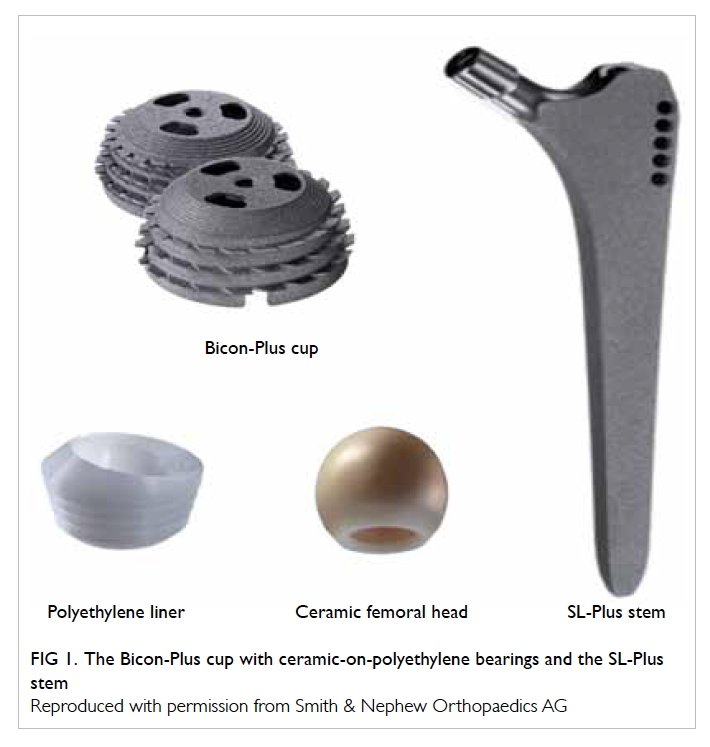
Figure 1. The Bicon-Plus cup with ceramic-on-polyethylene bearings and the SL-Plus stem
Reproduced with permission from Smith & Nephew Orthopaedics AG
Perioperative care
All THAs were performed by the senior surgeon
(BL Kou) through a modified Hardinge direct lateral
approach. The mean (± standard deviation) desired
acetabular position was 45° ± 10° of abduction and 15°
± 10° of anteversion, the femoral position was 5°-10°
of anteversion: both were evaluated by postoperative
X-ray. In order to facilitate optimal insertion of the
bone, the bone had to be shaped to the Bicon-Plus
cup by matched directional devices. All patients
received prophylactic antibiotics prior to surgery
and subcutaneous low-molecular-weight heparin
calcium for prophylaxis against thrombosis for 2
weeks postoperatively. Patients were discharged after
a mean of 5 days after surgery. Mobilisation with full
weight-bearing was encouraged the day after surgery.
At postoperative 6 weeks, rehabilitation exercises
were commenced and the hip joint mobilised.
Clinical and radiological assessment
The Harris Hip score (HHS),10 which is a disease-specific
health-related quality-of-life instrument
and widely used to evaluate physical function and
pain relief in patients with various hip diseases, was
used to clinically evaluate patients preoperatively,
postoperatively, and at the most recent follow-up.
Anteroposterior and lateral supine radiographs of
the hip and femur were analysed for radiolucencies,
osteolysis, and migration of the components, and
compared with radiographs taken 2 weeks after
surgery. Osteolytic areas and radiolucencies adjacent
to the SL-Plus and Bicon-Plus were evaluated using
the zones described by Gruen et al11 and DeLee and
Charnley,12 respectively. Osteolysis was described as
a sharply demarcated radiolucent space with rounded
or scalloped appearance that was >2 mm wide.13 The
migration of the cup was defined as movement of
≥3 mm in a horizontal or vertical direction and stem
migration was defined as a change in position of
>4 mm relative to the mid-lesser trochanter. Femoral
implant stability was assessed by the radiographs
according to the criteria of Engh et al,14 as stable
with osseointegration or fibrous tissue ingrowth, or
as unstable. Heterotopic ossification was evaluated
using the criteria described by Brooker et al.15 Liner
wear was determined by subtracting the thickness
of the polyethylene on the first radiograph of the
hip postoperatively in the standing position from
the last available control radiograph corrected for
enlargement and determined in relation to the
diameter of the head component.15 We only included
cases of annual liner wear of >0.1 mm/year due to
the lack of precision of these measurements.
Statistical analysis
Demographic and X-ray variables were assessed
with descriptive statistics. Kaplan-Meier survival
analyses16 with 95% confidence intervals (CI) were
used to determine the survival rate with the use
of several end-points: revision for any reason or
revision for aseptic loosening for each component
of the THA system. All patients were included in
the Kaplan-Meier analysis. Patients who died were
censored at their date of death and patients who
were lost to follow-up were censored at the date of
last assessment. Continuous variables of HHS were
compared using a two-sided Student’s t test. The
Statistical Package for the Social Sciences (Windows
version 19.0; IBM Corp, Armonk [NY], United States) was used
to analyse the collected data. A P value of <0.05 was
considered significant.
Results
Sample
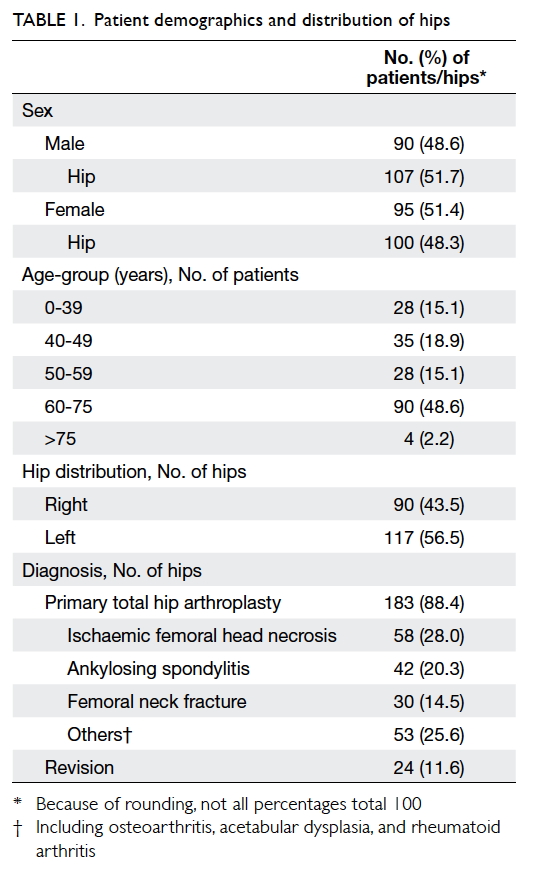
Demographic data of patients and indications for
implantation of the prosthesis are listed in Table 1. There were 95 women and 90 men, and the mean age
(± standard deviation) at the time of the index surgery
was 57.8 ± 13.8 years (range, 16-72 years). Overall,
161 patients (183 hips) underwent primary THA
only and the most common indication was ischaemic
femoral head necrosis (58 hips). Other indications
included ankylosing spondylitis and femoral neck
fracture (Table 1). Another 24 hips underwent surgery for revision (15 for aseptic loosening, 6 for
migration of the acetabular component, and 3 for
deep infection) and the mean time between the
primary THA and this revision was 3.2 years.
Follow-up
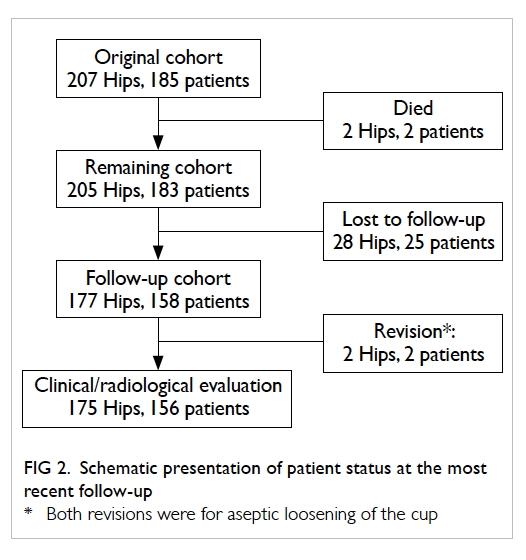
As shown in Figure 2, two patients (two hips)
died without a revision prior to death for reasons
unrelated to the surgery; the time between operation
and death were 4.2 years and 5.1 years, respectively. Twenty-five
patients (28 hips) were lost to follow-up. The main
cause for patients lost to follow-up was change
of residence and/or phone number. Revision was
performed in two patients (two hips). A total of 156
patients (175 hips) were available for clinical and
radiological evaluation, with a mean time between
operation and final evaluation of 14.1 years (range, 12.4-16.5 years).
Revisions
There were two (0.97%) revisions in the whole series
of 207 hips. An example of good results at 16.5 years
of follow-up is shown in Figure 3. The stem alone had not been revised in any hip. The Bicon-Plus cup alone had
been revised in two hips, both for aseptic loosening.
Radiographs of aseptic loosening of acetabular
components before and after revision at 10.7 years
until the latest follow-up are shown in Figure 4. Both revision surgeries were performed on men after 10.7
and 16.5 years postoperatively. No perioperative
complications were observed after revision and the
HHS were 92 and 96 post-revision, respectively.
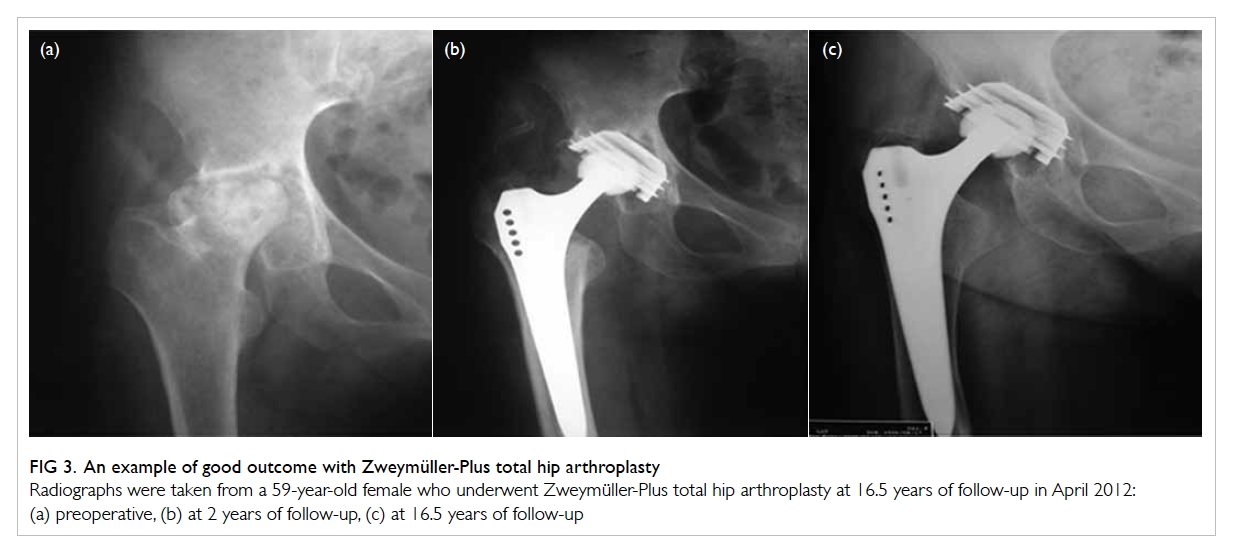
Figure 3. An example of good outcome with Zweymüller-Plus total hip arthroplasty
Radiographs were taken from a 59-year-old female who underwent Zweymüller-Plus total hip arthroplasty at 16.5 years of follow-up in April 2012: (a) preoperative, (b) at 2 years of follow-up, (c) at 16.5 years of follow-up
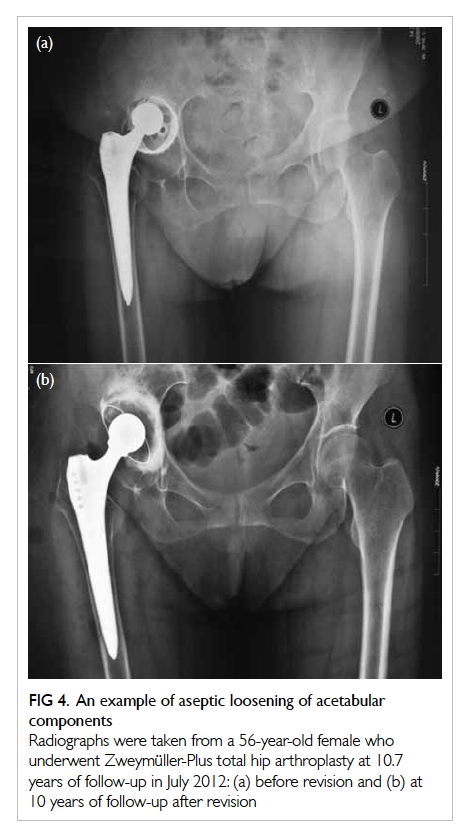
Figure 4. An example of aseptic loosening of acetabular components
Radiographs were taken from a 56-year-old female who underwent Zweymüller-Plus total hip arthroplasty at 10.7 years of follow-up in July 2012: (a) before revision and (b) at 10 years of follow-up after revision
There were no other re-operations at the time
of most recent follow-up. Two hips (two patients),
however, showed excessive polyethylene wear of
the liner although both were asymptomatic. Liner
exchange was recommended but both patients
refused. They were closely monitored for observation
of wear progression and osteolysis development.
Radiological evaluation of surviving hips
Non-progressive radiolucent lines around the
femoral component (<1 mm) were found in seven
(4.0%) of 175 stems, all limited to the proximal
femur (Gruen zone 7). Comparison of early and
late postoperative radiographs revealed no signs of
osteolysis in the distal femoral zones or subsidence
of femoral prosthesis of >1 mm. Intramedullary
ossification was found in five (2.9%) of 175 stems.
There was no excessive liner wear in the remaining
173 hips.
Non-progressive radiolucent lines of <2 mm
were found around the Bicon-Plus cup in three (1.7%) of
175 hips in DeLee-Charnley zone III. No extensive
peri-acetabular osteolysis radiographically of >2 mm
was observed in any hip. Heterotopic ossification was
found in 23 (13.1%) of 175 hips with various degrees
according to the criteria by Brooker et al.15 Among
the 23 hips, 11 hips were considered Brooker grade I,
eight hips were Brooker grade II, and the remaining
four were Brooker grade III.
Clinical evaluation of surviving hips
A total of 156 patients (175 hips) were available
for clinical and radiological evaluation. The
mean HHS for the 175 hips increased significantly
from 39.3 ± 3.8 preoperatively to 94.1 ± 2.5 postoperatively at a mean follow-up of 14.1 years (P<0.05).
Complications
Intra-operative complications including pulmonary
and deep vein thrombosis were not observed in
any patient. Surgical complications including
calcar cracks, femoral fracture, deep infection, and
dislocation did not occur in any patient. In addition,
no medical complications were observed in cardiac,
urinary, or psychiatric aspects.
Survival analysis
The Kaplan-Meier survival analysis, with the
end-point being revision of any component for any
reason, estimated the 14.1-year (minimum follow-up
of 12.4 years) survival rate at 99.03% (95% CI, 95%-100%). Since the reason for
both revisions was aseptic loosening of the Bicon-cup,
the survival rate at a minimum of 12.4 years
of follow-up with removal of any component for
aseptic loosening and the probability of survival of
acetabular components with revision for any reason
were both 99.03% (95% CI, 95%-100%). In addition,
the survival rate of the SL-Plus stem with revision for
any reason was 100%. The worst case survival of this
ceramic-on-polyethylene THA, when taking the two
pending revision cases into account, with removal of
any component for any cause as the end-point was
98.07% (95% CI, 84%-100%).
Discussion
Medium- to long-term follow-up studies are
required to evaluate the effectiveness of orthopaedic
implants in patients with various hip diseases. The
present study was conducted in a group of 207 hips
after a mean follow-up of 14.1 years to evaluate the
medium-term effectiveness of the Zweymüller-Plus
THA with ceramic-on-polyethylene bearings.
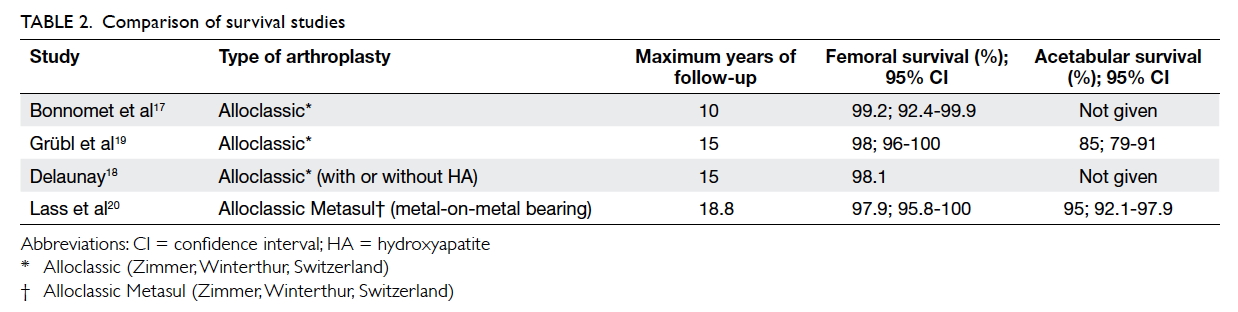
The main finding of this study was the
relatively high survival rate of both implant
components (100% for the femoral component and
99.0% for the acetabular component). The worst
survival when taking the pending revisions into
account was still 98.1%. Although methodological
differences and dissimilar implant designs can limit
comparison of different THAs, the survival rate
of the stem and cup in our series is comparable or
even higher than previous descriptions for other
THAs, especially the Alloclassic system (Zimmer,
Winterthur, Switzerland). Bonnomet et al17 reported
that the 10-year survival with stem revision for any
reason as the end-point of the Alloclassic-SL grit-blasted
titanium stem in primary THA was 99.2%.
For Alloclassic THAs with/without hydroxyapatite coating on the fixation of a cementless
femoral stem, the 15-year survival of the stem for
the event (revision for any reason) was 98.1%.18 For
another cementless Zweymüller-Alloclassic system,
a survival rate of 98% for the stem and 85% for the
cup at 15 years with revision for any reason as the
end-point has been reported.19 Femoral survival and
acetabular survival with the Alloclassic system are
shown in Table 2.17 18 19 20 Consistent with our results, long survival of Zweymüller-Plus components
with ceramic-on-polyethylene bearings has been
reported previously. A retrospective analysis
of results after a mean follow-up of 11 years by
Korovessis et al21 showed that the rate of survival
was 100% for the Bicon-Plus and 98% for the SL-Plus.
As a successor of the Alloclassic system, there
are several improvements in the Zweymüller-Plus
system. The sharp edges of the Alloclassic stem have
been rounded in the SL-Plus stem and this may avoid
distal stress concentration, cortical thickening, and
subsequent thigh pain.22 23 Moreover the Bicon-Plus
cup has inherent advantages over the Alloclassic cup
when implanted in hips with deficient or deformed
acetabulum since positioning of the biconical
threaded cup does not require removal of so much
spherical acetabular bone.21 All these features make
the Zweymüller-Plus system hypothetically practical
and stable.
The type of bearing couple may be the major
limitation for longevity of well-fixed hip implants.24
A previous comparison of four bearings revealed
that ceramic-on-polyethylene bearing couple
achieved the best results for revision for any reason
(98.1%).9 Similar to a previous description, the
survival of the ceramic-on-polyethylene bearings
in the Zweymüller-Plus system was relatively
high in our study (99.0%). Ceramic bearings have
several advantages over other bearings such as a
low coefficient of friction, low wear rates, and less
biologically reactive debris.25 26 27 They also have
several drawbacks such as susceptibility to fracture,28
although they avoid the adverse qualities associated
with polyethylene.9 In our study, there were no
revisions due to ceramic fracture.
The problems with polyethylene wear and
osteolysis are often considered to compromise the
long-term survival of implants. In an analysis based
on the Norwegian Arthroplasty Register, Hallan et al29 showed that high revision rates for polyethylene wear and osteolysis lead to an obvious decline in
survival after 10 years. There is an improvement
in osteolysis of the Alloclassic cup compared with
cemented polyethylene cups with ceramic-on-polyethylene
bearing surfaces, since radiolucent
lines and osteolysis in the Alloclassic cup were
evident in 0% to 6% of cases after 9.3 to 12 years19 30 while osteolysis around cemented cups was present
in 11% at 11.2 years.31 In our study, radiolucent lines
and osteolysis in the Bicon-Plus cups was 1.7%
at 14.1 years, which is lower than that in previous
reports.19 30 Additionally, the osteolysis and radiolucent lines were all located proximally and did not extend
around the distal part of the stem. The osteolysis rate
(4%) of the SL-Plus stem at 14.1 years was also lower.
Our findings were tempered by the limitations
inherent in our study design. The retrospective
design and the high number of patients lost to
follow-up might lead to excessively optimistic
results. In addition, patients who died or who were
lost to follow-up were not included in the clinical
analysis although their data were included in the
survival calculation to minimise the bias. Despite
these limitations, our study with a relatively long
follow-up and a large number of patients provides
evidence of the clinical durability of the ceramic-on-polyethylene
Zweymüller-Plus THA.
Conclusions
Our results indicate that the Zweymüller-Plus system
with ceramic-on-polyethylene bearing showed a
long survival and durability at a mean follow-up of
14.1 years, along with an improvement in osteolysis
of both the SL-Plus stem and Bicon-Plus cup. Longer
follow-up is still necessary to monitor the long-term
outcomes for the Zweymüller-Plus system with
ceramic-on-polyethylene.
Declaration
The authors declare that they have no competing interests.
References
1. Schulte KR, Callaghan JJ, Kelley SS, Johnston RC. The
outcome of Charnley total hip arthroplasty with cement
after a minimum twenty-year follow-up. The results of one
surgeon. J Bone Joint Surg Am 1993;75:961-75. Crossref
2. Severt R, Wood R, Cracchiolo A 3rd, Amstutz HC. Long-term
follow-up of cemented total hip arthroplasty in
rheumatoid arthritis. Clin Orthop Relat Res 1991;(265):137-45. Crossref
3. Hailer NP, Garellick G, Kärrholm J. Uncemented and
cemented primary total hip arthroplasty in the Swedish
Hip Arthroplasty Register. Acta Orthop 2010;81:34-41. Crossref
4. Repantis T, Vitsas V, Korovessis P. Poor mid-term survival
of the low-carbide metal-on-metal Zweymüller-Plus
total hip arthroplasty system: a concise follow-up, at a minimum
of ten years, of a previous report. J Bone Joint Surg Am
2013;95:e331-4. Crossref
5. Goldring SR, Clark CR, Wright TM. The problem in total
joint arthroplasty: aseptic loosening. J Bone Joint Surg Am
1993;75:799-801. Crossref
6. Harris WH. Wear and periprosthetic osteolysis: the
problem. Clin Orthop Relat Res 2001;(393):66-70. Crossref
7. Petsatodis GE, Papadopoulos PP, Papavasiliou KA,
Hatzokos IG, Agathangelidis FG, Christodoulou AG.
Primary cementless total hip arthroplasty with an alumina
ceramic-on-ceramic bearing: results after a minimum
of twenty years of follow-up. J Bone Joint Surg Am
2010;92:639-44. Crossref
8. Korovessis P, Petsinis G, Repanti M, Repantis T. Metallosis
after contemporary metal-on-metal total hip arthroplasty.
Five to nine-year follow-up. J Bone Joint Surg Am
2006;88:1183-91. Crossref
9. Topolovec M, Miloev I. A comparative study of four
bearing couples of the same acetabular and femoral
component: a mean follow-up of 11.5 years. J Arthroplasty
2014;29:176-80. Crossref
10. Davis KE, Ritter MA, Berend ME, Meding JB. The
importance of range of motion after total hip arthroplasty.
Clin Ortho Relat Res 2007;465:180-4.
11. Gruen TA, McNeice GM, Amstutz HC. “Modes of
failure” of cemented stem-type femoral components: a
radiographic analysis of loosening. Clin Ortho Relat Res
1979;(141):17-27.
12. DeLee JG, Charnley J. Radiological demarcation of
cemented sockets in total hip replacement. Clin Ortho
Relat Res 1976;(121):20-32.
13. Zicat B, Engh CA, Gokcen E. Patterns of osteolysis around
total hip components inserted with and without cement. J
Bone Joint Surg Am 1995;77:432-9. Crossref
14. Engh CA, Bobyn JD, Glassman AH. Porous-coated hip
replacement. The factors governing bone ingrowth,
stress shielding, and clinical results. J Bone Joint Surg Br
1987;69:45-55.
15. Brooker AF, Bowerman JW, Robinson RA, Riley LH Jr.
Ectopic ossification following total hip replacement.
Incidence and a method of classification. J Bone Joint Surg
Am 1973;55:1629-32. Crossref
16. Kaplan EL, Meier P. Nonparametric estimation from
incomplete observations. J Am Stat Assoc 1958;53:457-81. Crossref
17. Bonnomet F, Delaunay C, Simon P, et al. Straight femoral
taper in cementless primary total hip replacement in
less than 65 year-old patients: multicenter study of 115
consecutive implantations at mean 8.2 year follow-up
[in French]. Rev Chir Orthop Reparatrice Appar Mot
2001;87:802-14.
18. Delaunay C. Effect of hydroxyapatite coating on the radio-clinical
results of a grit-blasted titanium alloy femoral
taper. A case-control study of 198 cementless primary
total hip arthroplasty with the Alloclassic system. Orthop
Traumatol Surg Res 2014;100:739-44. Crossref
19. Grübl A, Chiari C, Giurea A, et al. Cementless total hip
arthroplasty with the rectangular titanium Zweymüller
stem. A concise follow-up, at a minimum of fifteen years,
of a previous report. J Bone Joint Surg Am 2006;88:2210-5. Crossref
20. Lass R, Grübl A, Kolb A, et al. Primary cementless total
hip arthroplasty with second-generation metal-on-metal
bearings: a concise follow-up, at a minimum of
seventeen years, of a previous report. J Bone Joint Surg Am
2014;96:e37. Crossref
21. Korovessis P, Repantis T, Zafiropoulos A. High medium-term
survivorship and durability of Zweymüller-Plus total
hip arthroplasty. Arch Orthop Trauma Surg 2011;131:603-11. CrossRef
22. Grübl A, Chiari C, Gruber M, Kaider A, Gottsauner-Wolf F. Cementless total hip arthroplasty with a tapered, rectangular titanium stem and a threaded cup: a minimum
ten-year follow-up. J Bone Joint Surg Am 2002;84-A:425-31. CrossRef
23. Garcia-Cimbrelo E, Cruz-Pardos A, Madero R, Ortega-Andreu M. Total hip arthroplasty with use of the cementless Zweymüller Alloclassic system. A ten to thirteen-year
follow-up study. J Bone Joint Surg Am 2003;85-A:296-303. CrossRef
24. Zywiel MG, Sayeed SA, Johnson AJ, Schmalzried TP, Mont
MA. State of the art in hard-on-hard bearings: how did
we get here and what have we achieved? Expert Rev Med
Devices 2011;8:187-207. Crossref
25. Murphy SB, Ecker TM, Tannast M. Two-to 9-year clinical
results of alumina ceramic-on-ceramic THA. Clin Orthop
Relat Res 2006;453:97-102. Crossref
26. Affatato S, Traina F, De Fine M, Carmignato S, Toni
A. Alumina-on-alumina hip implants: a wear study of
retrieved components. J Bone Joint Surg Br 2012;94:37-42. Crossref
27. Revell PA. The combined role of wear particles,
macrophages and lymphocytes in the loosening of total
joint prostheses. J R Soc Interface 2008;5:1263-78. Crossref
28. Park YS, Hwang SK, Choy WS, Kim YS, Moon YW, Lim
SJ. Ceramic failure after total hip arthroplasty with an
alumina-on-alumina bearing. J Bone Joint Surg Am
2006;88:780-7. Crossref
29. Hallan G, Dybvik E, Furnes O, Havelin LI. Metal-backed
acetabular components with conventional polyethylene: a
review of 9113 primary components with a follow-up of 20
years. J Bone Joint Surg Br 2010;92:196-201. Crossref
30. Perka C, Fischer U, Taylor WR, Matziolis G. Developmental
hip dysplasia treated with total hip arthroplasty with a
straight stem and a threaded cup. J Bone Joint Surg Am
2004;86-A:312-9. Crossref
31. Sugano N, Nishii T, Nakata K, Masuhara K, Takaoka
K. Polyethylene sockets and alumina ceramic heads in
cemented total hip arthroplasty. A ten-year study. J Bone
Joint Surg Br 1995;77:548-56.